Up to 24% Of Women With Urinary Incontinence Have Fecal Incontinence1
Fecal Incontinence – The Condition No-One Wants to Talk About
Fecal incontinence (FI) is the uncontrolled leakage of fecal matter (poop/stool) or gas. This can be solid stools or stools that have been liquidized (diarrhea) as well as gas. FI is one of the most debilitating symptoms of all pelvic floor dysfunctions. The psychological impact is dramatic and if you suffer this condition, you may be reluctant to report your symptoms or to seek help. Even healthcare providers can be reluctant to enquire about this condition, which can leave you feeling lost and alone. Embarrassment and shame can hinder you from finding the help you need. This further emphasises the importance of the #BreakthePFDtaboo campaign.
Symptoms and Cause of Fecal Incontinence
The main symptom of fecal incontinence is leakage of stool. It is generally caused by weakness of the anal sphincter muscle. If you become sick and develop severe diarrhea, you may experience the unintentional leakage of runny poo, however this is not considered fecal incontinence but rather a symptom of your sickness. If the leakage continues once your illness has cleared, this could indicate fecal incontinence, where leakage happens under “normal” conditions in the absense of illness.
I Fart a Lot, Does That Mean I Have Fecal Incontinence?
Flatulence (where you are unable to control your gas) is considered to be a form of fecal incontinence if it is caused by weakness of the anal sphincter. Let’s imagine that you are in a job interview. If you are unable to hold in your gas in that situation (when farting is not considered appropriate), this could indicate sphincteric weakness.
The average person farts 14 times per day, and for some people it can be a lot more, but farting a lot does not mean that you have fecal incontinence. It is the inability to hold in a fart at an inopportune moment that highlights you may have some inefficiency in your external anal sphincter. When FI becomes more severe, leakage can be anything from a small amount of poop to complete emptying of the bowel. There is a high prevalence of depression amongst women with FI with many claiming to “succumb” to the condition. We don’t want you to succumb, we want you to fight back and regain control, and to know that you are not alone.
Over 40% Of Adults Referred for Anorectal Physiological Investigation Had Coexistent Diagnoses of Fecal Incontinence and Functional Constipation2
The Process of Defecation (Pooping)
Your anus is the end of a long pipe that runs from your mouth to your bottom. In between your mouth and your bottom, the food you eat gets broken down by billions of microbes (bacteria) that are part of your microbiome which forms a large part of your immune system. Food is moved by the smooth muscle that forms the digestive tract (stomach, intestines etc). By the time the food you have eaten makes it to your rectum, it has been heavily processed by your digestive system, leaving waste (mostly fibre and substances that cannot be digested). Your pelvic floor creates a barrier to prevent your poop from coming straight out of your body, allowing it to accumulate into a sufficient “poop-sausage” before initiating the reflex that lets you know its time to empty (intrinsic myenteric defecation reflex). This first reflex moves the poop towards your anus letting you know, poo time is here. Your external anal sphincter is responsible for holding the anus closed.
The Role of the Pelvic Floor in Defecation
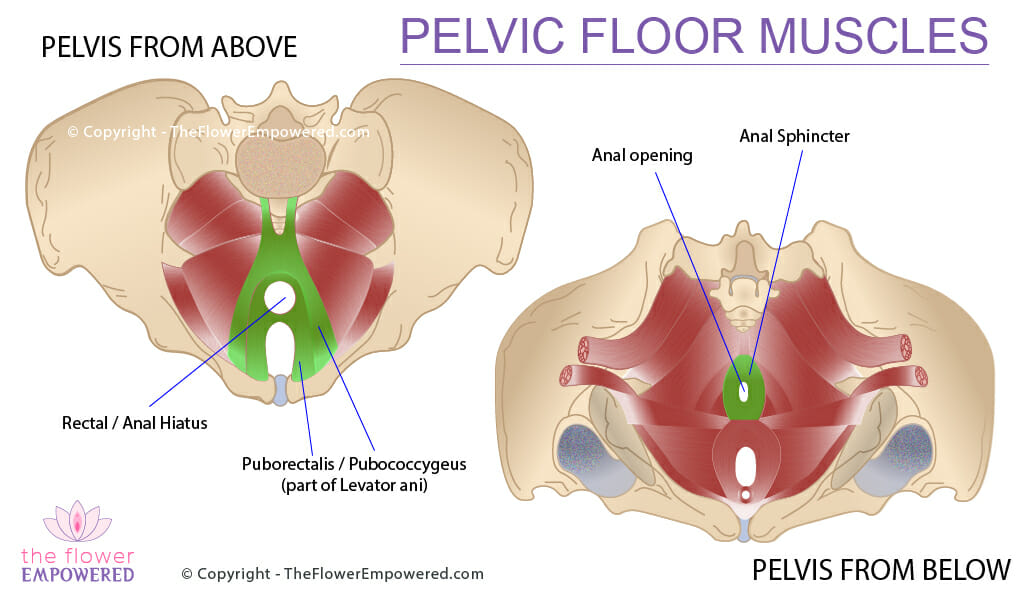
The intrinsic myenteric defecation reflex moves your poop towards your external anal sphincter, however, it meets with the resistance of your pelvic floor, more specifically the puborectalis muscle which is part of your Levator ani. This muscle puts a kink in your rectum which slows the decent of poop that is headed towards the exit (your anus). This kink creates the anorectal angle. The external anal sphincter should hold the rectum closed until the stretch receptors in the rectum trigger the urge to empty.
Of course, just like the process of urination, you learned as a child to control the external anal sphincter allowing you to hold your poop until a toilet could be found. Once a toilet is found, you squat down (hopefully!), relaxing your external anal sphincter and allowing the poop to exit the body. In the book, we explore the process of defecation in more detail to gain valuable insights which are utilised in the whole life, whole mind, whole body approach to rehabilitation.
How Does Fecal Incontinence Occur?
FI is a complex condition with many impacting factors, so let’s focus solely on the role of pelvic floor. The mechanism of continence is dependent on both the puborectalis (which creates a kink in the rectum), and the external anal sphincter, both of which are under your voluntary control. Weakness in the pelvic floor can result in laxity and atrophy of these and other muscles of the pelvic floor.
A weak pelvic floor typically sit lower providing less support for the organs of the pelvis (bladder, uterus and rectum). If you have read the urinary incontinence and pelvic organ prolapse pages, you will be familiar with the impact of weak pelvic floor muscles. In respect of the puborectalis and levator ani, weakness results in a decrease in the anorectal angle. This can increase the risk of FI as a reduction in this angle allows more, if not all of the fecal content to weigh down on the external urethral sphincter. This reduction in angle is important when you need to poo. Squatting to poo reduces the angle significantly allowing for a faster evacuation.
Weakness in the external anal sphincter is the real killer though. The external anal sphincter needs to have sufficient strength to hold tightly closed. You have voluntary control of the muscle so when it is sufficient in strength, you can maintain the closure. Lack of strength means that the pressure of feces bearing down will be greater than the pressure holding the muscle closed. This will result in a leakage.
The muscle can be weak due to atrophy, or in many cases, it can be weak due to injury. If tearing during childbirth is severe, this can cause a sphincter tear. Depending on the quality of repair and on the subsequent muscle rehabilitation, you will have more or less strength in this muscle. Sometimes fecal incontinence can occur after the bowel has been emptied, if it had failed to empty fully. This can happen due to a rectocele, where weakness in the pelvic floor and the back vaginal wall (posterior) allows the rectum to prolapse into the vagina. You can read more on rectocele and treatments in the pelvic organ prolapse section of the knowledge portal.
How Can I Know the Severity of My Fecal Incontinence (FI)?
Unlike urinary incontinence with the Sandvik Test, there is currently no standard qualification method to define the severity of FI. For this reason, we have created an adapted version of the Sandvik Test to help you assess the severity of your FI. When you meet with a pelvic health specialist, you can share your results with them.
Products for Management of Fecal Incontinence
There are many products that can be used in the management fecal incontinence. We have include some of those products below. You should speak with your pelvic floor physiotherapist or doctor before using these products. Reviews of these products will be covered on our YouTube channel. If there is a specific product that you would like to see reviewed, just get in touch and we will review. Note that these products have affiliate links. Should you choose to purchase them, we will make a small commission.
Incontinence Pants
Anal Probe
Innovo E-Stim Shorts
Treatment Options for Fecal Incontinence
Like most symptoms of pelvic floor dysfunction, the treatment for fecal incontinence falls into one of two categories; conservative (non-surgical) and invasive (surgical). Surgical options are generally only advised for once conservative options have been tried unsuccessfully for an extended period. For more information on the various treatments offered in these two categories, click on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
References
- Markland AD, Richter HE, Kenton KS, Wai C, Nager CW, Kraus SR, Xu Y, Tennstedt SL; Urinary Incontinence Treatment Network. Associated factors and the impact of fecal incontinence in women with urge urinary incontinence: from the Urinary Incontinence Treatment Network’s Behavior Enhances Drug Reduction of Incontinence study. Am J Obstet Gynecol. 2009 Apr;200(4):424.e1-8. doi: 10.1016/j.ajog.2008.11.023. Epub 2009 Feb 6. PMID: 19200939; PMCID: PMC2692265.
- Vollebregt PF, Wiklendt L, Dinning PG, Knowles CH, Scott SM. Coexistent faecal incontinence and constipation: A cross-sectional study of 4027 adults undergoing specialist assessment. EClinicalMedicine. 2020 Oct 13;27:100572. doi: 10.1016/j.eclinm.2020.100572. PMID: 33150331; PMCID: PMC7599308.