15.1 % Of Us Women Report OAB1
What Is Overactive Bladder (OAB) And What Are the Symptoms?
Overactive Bladder is a condition where there is a frequent need to urinate. The average adult female urinates up to 8 times per day. If you are urinating more frequently than this, your bladder may to be overactive. The condition can manifest with symptoms such as urgency to urinate, urge incontinence (UUI), frequency incontinence and nocturia (needing to pee multiple times during the night). Any combination of these symptoms can be a sign of an overactive bladder. Those who suffer from OAB need to know where the bathroom is at all times and even then, there is a risk they won’t make it. It can be difficult or impossible to control the urge. Unlike stress incontinence, OAB is not triggered by exertion.
What Causes Overactive Bladder?
Whereas the exact cause is not implicitly known, it is believed to be more neurologic in nature. Episodes of overactive bladder can be triggered by factors such as excessive coffee or alcohol consumption. Age is also a contributing factor, however overactive bladder should not be considered a normal sign of ageing. Excess tension in the pelvic floor muscles can trigger urgency, so pelvic floor relaxation exercises often help to relieve the symptoms. Overactive bladder is clinically defined as an overactive bladder in the absence of any of any pathology (disabilities, illnesses, infections or injuries that can cause OAB symptoms).
If you suffer from multiple sclerosis (MS) or have a spinal cord injury, you may suffer the same symptoms as OAB, however, Reflex incontinence (neurogenic bladder) is the term given in this case. Functional incontinence also produces similar symptoms to OAB but is unrelated to your bladder and urinary tract, for example, if you have Alzheimer’s, Parkinson’s or have a stroke. Function incontinence is also the term used to describe incontinence caused by conditions that produce excessive urine such as diabetes. Functional incontinence can also be a side effect of infection, medication or medical treatment. You can read more on Function and reflex incontinence on the page for those conditions.
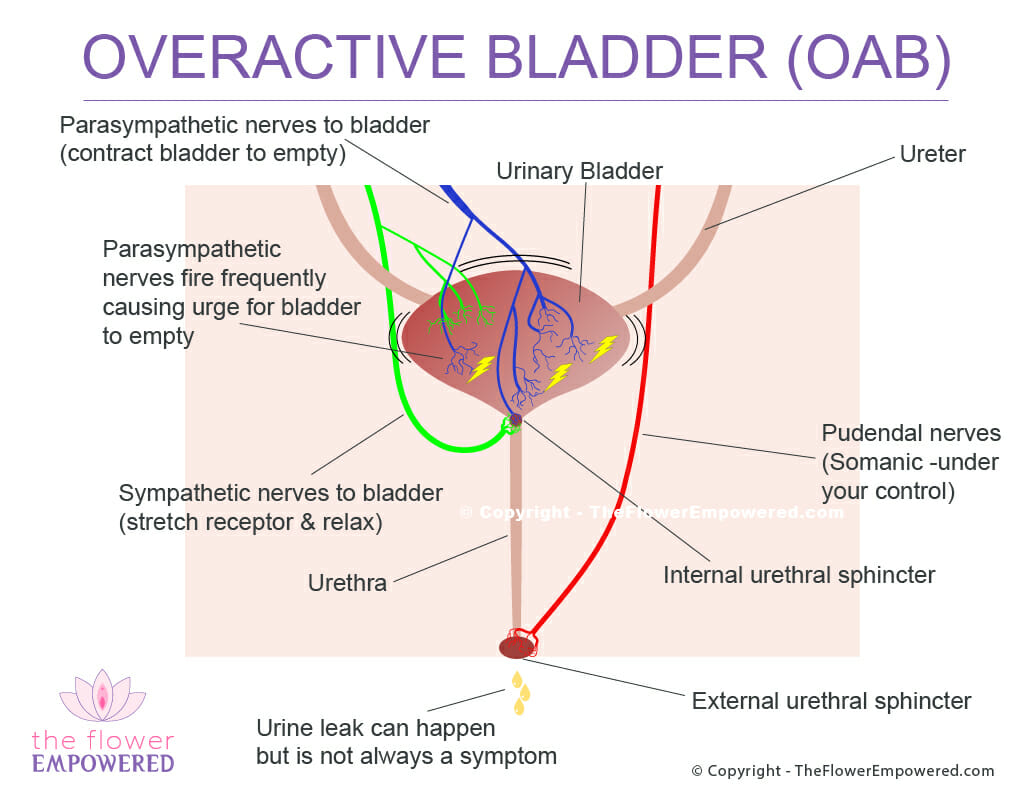
Overactive Bladder Explained
We’ve created the image to show what happens when you have an overactive bladder. The small yellow electric shock’s on the image attempt to convey the nerves signals triggering the bladder to empty.
Your bladder slowly fills as your kidneys send urine through the ureters to the bladder.
Stretch receptors are monitoring the urine in your bladder while simultaneously keeping the bladder muscle relaxed.
Parasympathetic nerves trigger prematurely causing the bladder to contract sending urine through the urethra.
As the bladder contracts, extreme urge is felt. In some cases, leakage can occur. This can be anything from a few drops to full bladder leakage.
Does Peeing “Just in Case” Cause OAB?
Just in case (JIC) peeing can be viewed as a way to negatively reprogram your bladder. If you JIC pee, you will change how your nervous system interprets the volume of urine in your bladder. This can result in an increase in your frequency of urination; therefore you will pee smaller amounts more frequently. Over time, this can impact your bladder function as your sensitive stretch receptions become unfamiliar with the feeling of a full bladder.
When you are potty trained as a child, you learn to read your body’s guarding reflex to hold your urine until got to the bathroom. This was a positive programming of your bladder function. It is possible to reprogram your bladder function in the same way, which is known as bladder retraining, which is covered in the conservative treatments page.
11.0 % of Women Report OAB With Urge Urinary Incontinence1
Products for Management of Overactive Bladder
There are many products that can be used in the management overactive bladder. We have include some of those products below. You should speak with your pelvic floor physiotherapist or doctor before using these products. Reviews of these products will be covered on our YouTube channel. If there is a specific product that you would like to see reviewed, just get in touch and we will review. Note that these products have affiliate links. Should you choose to purchase them, we will make a small commission.
Treatment Options for Urinary Incontinence
Like most symptoms of pelvic floor dysfunction, the treatment for urinary incontinence falls into one of two categories; conservative (non-surgical) and invasive (surgical). Surgical options are generally only advised for once conservative options have been tried unsuccessfully for an extended period. For more information on the various treatments offered in these two categories, click on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
Explore the Other Types of Urinary Incontinence
Having reviewed overactive bladder, you may be interested in exploring the other types of incontinence. You can do that from here:
References
- Reynolds WS, Fowke J, Dmochowski R. The Burden of Overactive Bladder on US Public Health. Curr Bladder Dysfunct Rep. 2016 Mar;11(1):8-13. doi: 10.1007/s11884-016-0344-9. Epub 2016 Jan 23. PMID: 27057265; PMCID: PMC4821440.