Surgical or obstetric trauma may lead to muscular pain with hypertonicity of the pelvic floor.1
The Nightmare of Pelvic Pain
Pelvic pain is a debilitating condition that negatively impacts your quality of life. 2% of the female population suffers from chronic pelvic pain symptoms, the causes of which are so varied that finding the root of the issue is not easy. This site is focused on pelvic floor dysfunction, so for this page, we will focus specifically on condition of hypertonicity, which is sometimes referred to as non-relaxing pelvic floor dysfunction (NR-PRD), hypertonic PFD, or levator ani syndrome (LAS). You can read more about hypertonicity on the pelvic floor dysfunction page.
It is critical to have any pain conditions investigated by your doctor. There are many pelvic pain conditions that fall outside of the scope of this website. We have listed some of these conditions below along with links to webpages that focus specifically on each of those conditions:
- Endometriosis – Almost 20% of women who undergo an investigation for pelvic pain are diagnosed with Endometriosis, which is a debilitating condition in which tissue, that normally lines the womb, grows outside the uterus (commonly on fallopian tubes or ovaries). It can cause adhesions or scar tissue. Symptoms include painful periods (dysmenorrhea), painful intercourse and excessive bleeding (Menorrhagia).
- Interstitial Cystitis (IC) – also known as painful bladder. This is a chronic condition where cystitis is present almost all the time. The symptoms of cystitis include a strong and persistent urge to pee, burning sensation when urinating and only passing a small amount at a time. Symptoms can also include blood in the urine, pelvic pain and sometimes a fever.
- Polycistic Ovary Syndrome (PCOS) – This is a hormonal condition that causes excess production of male hormones resulting in cysts on the ovaries. Other symptoms can include irregular or heavy periods, weight gain, excess body hair and skin conditions.
- Irritable Bowel Syndrome (IBS) – this condition is a chronic condition of the digestive system. Typical symptoms are cramps, bloating, diarrhoea and/or constipation.
- Menorrhagia (heavy periods) – this condition is not always accompanied by pelvic pain, however, it can be a cause. with Menorrhagia, periods are very heavy and tend to last longer than a week. It is normal to have to wake during the night to change sanitary protection.
- Pelvic Congestion Syndrome – this condition is believed to be caused by varicose veins in the pelvis. It causes chronic pelvic pain
- Chronic pelvic pain can also have many other causes. You can read more on the Pelvic Pain Support Network.
Why Does Pelvic Floor Hypertonicity Cause Pain?
Like any other muscles in the body, the pelvic floor can be hypertonic without pain, however, hypertonicity is often found when pain is present. The mechanism for pain from hypertonicity is not completely understood. It is believed to be impacted by excess tension. Pain can manifest in many different ways and can radiate to other areas. Pain can be constant or intermittent (for example, cramping in pelvic floor muscles following orgasm). The pelvic floor can have some muscles that are hypertonic (tight) and others that are hypotonic (lax/weak).
What Causes Pelvic Floor Hypertonicity
Hypertonicity can be caused by excess tension due to other conditions such as endometriosis, interstitial cystitis, polycystic ovary syndrome, irritable bowel syndrome, menorrhagia and pelvic congestion syndrome. Scarring from birth (especially following perineal repairs) and pelvic surgeries can also cause pelvic pain. Pelvic pain can increase stress and make you feel fearful, which activates the nervous systems “fight of flight” response, which in turn can add more tension. For this reason, it is important to reduce stress and practice relaxation if you are suffering from any pain condition.
Pelvic Pain Referral Patterns and Associated Symptoms
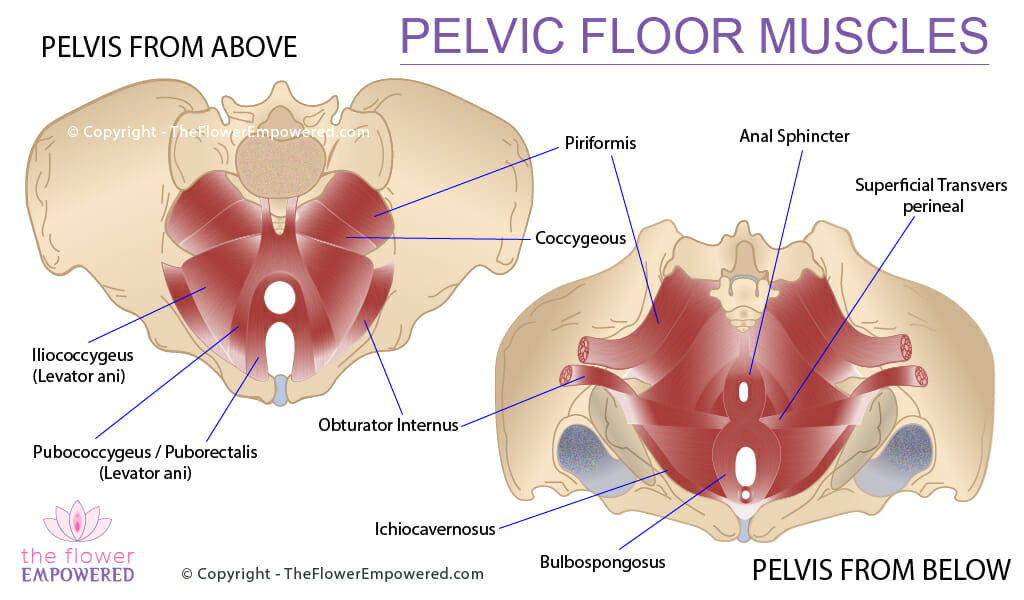
According to a 2012 study, referral patterns for pelvic pain from pelvic floor muscles are as follows:
| Pelvic Floor Muscle | Pelvic Pain Referral Pattern | Potential Symptom |
|---|---|---|
| Bulbospongosus | Perineal pain or urogenital pain | Painful sex, pain with orgasm or clitoral pain |
| Ischiocavernosus | Perineal pain or urogenital pain | Painful sex, pain with orgasm or clitoral pain |
| Superficial transverse perineal | None documented | Painful sex |
| Anal sphincter | Pain on posterior pelvic floor, rectum/anus or pubic pain | Burning or tingling in anus/rectum. Pain before, during or after pooping |
| Pubococcygeus / Puborectalis | Low-belly pain, bladder pain or pain in perineum | Increased urgency and/or frequency. Painful sex or painful urination after sex |
| Iliococcygeus | Pain towards the sacrum or deep in the vagina, rectum or perineum | Pain before, during or after pooping. Painful sex, particularly with thrusting |
| Coccygeous | Pain towards the sacrum or buttock pain | Pain on sitting. Pain during pooping. Intestinal fullness and anal pressure/pain |
| Obturator internus | Pain in anus, coccyx, vulva or vagina. Pain on back of thighs | Generalisd pelvic pain, often with burning or aching |
| Piriformis | Pain in sacrum, pain on one side of buttock | Buttock or leg pain. Sometimes sciatic pain |
After Completing Therapy, Patients With Chronic Pelvic Pain Used 22% Less Pharmacological Pain Relievers Compared to Patients Who Did Not Participate in Treatment.2
Hypertonic Does Not Mean Strong
Some people believe that hypertonic muscles are strong muscles, however, that is not generally the case. A hypertonic muscle will be in a constantly contracted state. When an increase in contraction is needed, which from the pelvic floor’s perspective would be when you cough (to prevent leakage) or when you orgasm, there won’t be any potential to increase contraction. This can mean that you leak urine (stress incontinence) or have weak orgasms.
Muscles that are hypertonic have less blood-flow which, over time, can result in atrophy (muscle breakdown). A healthy pelvic floor is one that can both contract and relax as needed, maintaining a balanced amount of tone under normal conditions. As well as stress incontinence, hypertonicity can sometimes exist with Overactive Bladder (OAB) which can be accompanied with urge incontinence. It is best to work with a pelvic floor physical therapist if you have hypertonicity, even if pain is not present.
Treatment Options for Pelvic Pain
Like most symptoms of pelvic floor dysfunction, the treatment for pelvic pain falls into one of two categories; conservative (non-surgical) and invasive (surgical). Surgical options are generally only performed as a treatment of other conditions. For more information on the various treatments offered in these two categories, click on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
References
- Grimes WR, Stratton M. Pelvic Floor Dysfunction. [Updated 2021 Jul 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559246/.
- Dydyk AM, Gupta N. Chronic Pelvic Pain. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554585/