11.1% Of Women With Symptomatic POP Will Require Surgery1
Invasive Treatments for Pelvic Organ Prolapse
When it comes to surgical treatments for pelvic organ prolapse, there are a number of alternatives available and the options presented to you will be dependent on your surgeon’s experience and preferences. There are two main types of pelvic organ prolapse surgery; Obliterative surgery and reconstructive surgery. Obliterative surgery narrows or closes the vaginal passage meaning intercourse is no-longer possible. This type of treatment is sometimes offered to elderly patients who are suffering severe pelvic organ prolapse symptoms and are no-longer sexually active. Reconstructive surgery, on the other hand, attempts to restore organs to their original position. This type of surgery can be preformed by open abdominal surgery, laparoscopic abdominal surgery or vaginal surgery. We will cover reconstructive surgeries on this page.
For reconstructive surgery, the actual procedure depends on the type and degree of prolapse. Surgical treatments for pelvic organ prolapse are not advised if you plan on having more children as pregnancy and childbirth will stretch the tissues which are nipped and tucked during repair. While you are still growing your family, it is best to use a pessary for POP management and focus on improving the strength of your pelvic floor. You can do PFMT both before and after your subsequent births and elect to have surgery when your pelvic floor is as strong as possible.
Graft or Native Tissue for Prolapse Repair
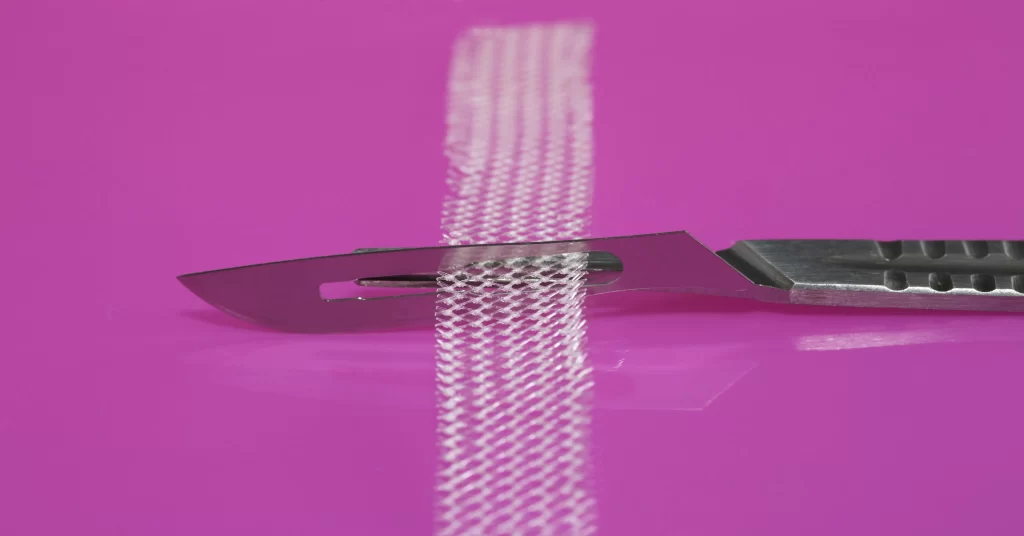
One of the key decisions to be taken when performing surgical repairs of pelvic organ prolapse is whether or not to use a graft material (mesh) or native tissue during the repair. The success rates for mesh and native tissue repairs are similar, but mesh adds additional risks of complications2. When using transvaginal mesh repair, there has been found to be a higher reoperation rate (11%) in comparison to native tissue repair (3.7%)3. The FDA (Food and Drug Association in USA) identified serious complications associated with the use of urogynecologic surgical mesh and as a result, many manufacturers removed their POP mesh repair products from the market.
Huge controversy exists around the use of mesh in the surgical repair of POP and bans are in place in many countries, although mesh is still offered in some countries. On this page, we will separate the surgical options into lower risk non-mesh surgeries and the higher-risk mesh surgeries. You need to remember that all surgeries carry risks, even those considered to be “minimally invasive” using native tissue. Carefully consider your options and make sure to get a second opinion if you are unsure.
Important Considerations Before Undergoing Pelvic Organ Prolapse Surgery
It is important to note that all surgeries carry risks and none have a 100% success rate. Surgery in the pelvic area has the potential to damage organs (bladder, uterus, bowel) as well as nerves, blood vessels and muscle/fascia. Following POP repairs, you could experience symptoms that you did not have prior to your surgery, such as stress incontinence (SUI) or overactive bladder (OAB). This new incontinence is referred to as “denovo incontinence”. Pelvic pain and sexual dysfunction can manifest following repairs.
The reported recurrence rate following surgical repairs vary greatly in studies with many reporting between 10 and 40%. Each surgery introduces the potential for injury as well as creating more scar tissue.
You should consider dedicating at least 18 months to conservative options before undertaking any surgery. Surgical repair will not make your pelvic floor stronger and there is no such thing as a quick-fix for pelvic organ prolapse. Following any pelvic floor surgery, you should work with your pelvic floor physical therapist to rehabilitate your pelvic which can help to mitigate any new symptoms.
Set Appropriate Expectations Before POP Repair Surgery
It is important to have realistic expectations if you are having surgery, and to ensure that your surgeon is aware of your expectations. What you believe to be surgical success might not be the same as your surgeons view of success. A 2010 study comparing the differing definitions for success following POP surgery found that great variations in definitions for success. The surgeon typically measures the objective cure rate, which is the anatomical cure (everything back in normal position), whereas the patient measures subjective cure rate – symptoms are alleviated and quality of life increases. How can these be different?
Let’s use a simple example: A patient has surgical repair for pelvic organ prolapse where a mesh graft is implanted. Following surgery, the pelvic organs are all back in their “normal” position, therefore she is objectively cured from the surgeons perspective. However, she now suffers from chronic hip pain and cannot have sex due to mesh eroding through her vagina. Although her pelvic organs are no-longer prolapsed, she views this surgery as unsuccessful due to the impact on her quality of life. Having frank and open discussions with your surgeon regarding your expectations and what they believe they can achieve with surgery can help to avoid these situations.
One Study Found Subjective Cure Rate for Vaginal Native Tissue Repair of Severe Prolapse Was 97.3% And the Objective Cure Rate Was 91.1%4
Native Tissue Surgical Treatments for Pelvic Organ Prolapse
In this section, we will review the native tissue surgical treatments for pelvic organ prolapse.
Anterior Vaginal Repair (Anterior Colporrhaphy)
An anterior vaginal repair (Anterior Colporrhaphy) is the primary treatment for cysotcele where the bladder prolapses through the front vaginal wall due to weakness of the tissues. In this procedure, both the connective tissues and vaginal wall on the front side are repaired using sutures.
If native tissues are insufficient, a biological graft can be used to provide extra support. Biological grafts can be either from a cadaver (allograft) or from animal derived collagen tissues (xenograft – typically from a cow or a pig). When using a biological graft, it will be soaked in an antibiotic solution prior to implantation. A 2004 study concluded that “in cases of high grade cystocele interposition of porcine dermis represents a successful and safe treatment option”.
Posterior Vaginal Repair (Posterior Colporrhaphy)
A posterior vaginal repair (Posterior Colporrhaphy) is the primary treatment for rectocele where the rectum prolapses through the back vaginal wall due to weakness of the tissues. In this procedure, both the connective tissues and vaginal wall on the back side are repaired using sutures.
A biological graft can be used to provide extra support if there is insufficient native tissue. These grafts can be either from a cadaver (allograft) or or animal derived collagen tissues (xenograft – typically from a cow or a pig). If a biological graft is used, it will be soaked in an antibiotic solution before implantation. A 2012 study into the use of surgisis (a graft from porcine intestine) concluded that surgisis “may decrease recurrences seen with native tissue repair and long-term complications of synthetic mesh. Its use in posterior compartment repair in particular is promising.”
This procedure is often accompanied by perineal repairs. The perineal repairs are required if the genital hiatus has increased in size (read more on the POP-Q page). The perineal body is an intersection for many of the muscles within the three layers of the pelvic floor playing an important role in their functional stability. Repair to the Perineal area involves reconnecting the muscles and connective tissues that converge around the perineum by suturing them back to their appropriate locations. Sometimes permanent sutures are used to hold things in place.
Uterosacral Ligament Suspension (Apical Repair)
Uterosacral ligament suspension is the primary treatment for uterine prolapse. The procedure is designed to restore support to the top of the vagina (apex). This also provides support for the uterus if present. A recent study highlighted that “its all about the apex” emphasising the importance of the uterosacral and cardinal ligaments in preventing POP.
In the absence of a uterus and if the Uterosacral ligament is unsuitable for some reason, a sacrospinous fixation is an alternative option. The image below shows approximate location of sutures for this type of repair. Some specialists argue that removal of the uterus compromises the support provided by these critical ligaments.
Sacrospinous Fixation (In Absence of Uterus)
Sacrospinous Fixation was first performed in 1968. The procedure is used to treat vaginal vault prolapse, enterocele or uterine prolapse (performed with a hysterectomy). This procedure is typically done in the absence of a womb. The vaginal vault is attached to the sacrospinous ligament either on one side only or bilaterally (both sides).
A 2018 study showed that patient questionnaires showed a significant improvement in sexual function with the bilateral sacrospinous fixation, with the greatest improvement being for the “Physical Factor”. Ileococcygeus Suspension is another similar procedure which attaches the vaginal vault to the fascia covering the Ileococcygeus muscle instead of the sacrospinous ligament. In the image, the vaginal vault has been attached to the sacrospinous ligament on the right side.
The concludes the surgical treatments with native tissue. We will now explore the options using mesh grafts.
In a Systematic Review, Vaginal POP Repair With Mesh Was Associated With a Summary Incidence of 10.3% Of Erosion5
Mesh Graft Surgical Treatments for Pelvic Organ Prolapse
In this section, we will review the surgical treatments for pelvic organ prolapse using synthetic mesh grafts. If you are offered a surgical repair using any graft that is not your own native tissue, you should be aware that those graft materials come with higher risks. The benefit of using these graft does not generally outweigh these risks.
In July 2011, the FDA released an update on Urogynecologic Surgical Mesh, specifically focusing on transvaginal placement for Pelvic Organ Prolapse. They determined that “(1) serious adverse events are NOT rare, contrary to what was stated in the 2008 PHN, and (2) transvaginally placed mesh in POP repair does NOT conclusively improve clinical outcomes over traditional non-mesh repair.”. They also highlighted that “Based on data from 110 studies including 11,785 women, approximately 10 percent of women undergoing transvaginal POP repair with mesh experienced mesh erosion within 12 months of surgery”. 10% equates to one in ten women. The FDA also recommended to health care providers that they “Recognize that in most cases, POP can be treated successfully without mesh thus avoiding the risk of mesh-related complications.”
Mesh manufacturers were told to provide proof of the efficacy and safety of Mesh for use in Pelvic Organ Prolapse. Their failure to do so resulted in the FDA ordering all manufacturers of surgical mesh to remove the devices from the market as they could not demonstrate the safety and effectiveness of mesh. NICE in the UK followed suit in June of 2019. If you are offered a graft other than your own native tissue for prolapse repairs, you should seek a second opinion.
Anterior Repair With Synthetic Mesh Graft
Anterior vaginal repair (Anterior Colporrhaphy) can sometimes require the use of a graft if native tissues are insufficient. Since its introduction to market, Synthetic mesh very quickly became the graft of choice, however, the common occurrence of complications resulted in many years of patient petitioning for mesh to be banned.
In April of 2019, almost 25 years after mesh was first used for these repairs, the US FDA announced that all mesh manufacturers should immediately stop selling and distributing their products. Just two months later in June 2019, NICE (the National Institute for Health and Care Excellence) in the UK issued similar guidelines. Many manufacturers have since removed mesh devices from the market but some are still used for laparoscopic repairs (abdominal placement).
It is important to note that synthetic mesh is a permanent implant. If you have issues with implantation, removal can leave substantial tissue damage and may require obliterative surgery.
There are several manufactures of mesh for POP repairs, the main ones being; J&J Ethicon, Boston Scientific, American Medical Systems, Bard and Coloplast.
Posterior Repair With Synthetic Mesh Graft
Posterior vaginal repair (Posterior Colporrhaphy) can sometimes require the use of a graft if your own native tissues are insufficient. Synthetic mesh has been the graft of choice for many years due to its low cost and speed of implantation, however, the very high rate of complications and negative side effects have resulted in the both the US FDA and the UK’s NICE pulling these meshes off the market.
It is important to note that synthetic mesh is a permanent implant. If you have issues with implantation, removal can leave substantial tissue damage and may require obliterative surgery.
Sacrocolpopexy With Mesh Graft
Sacrocolpopexy is a procedure to restore support to the top of the vaginal vault (apex) following hysterectomy. Sacrohysteropexy is the same procedure but with the uterus still in place. These procedures use synthetic mesh which has been removed from both the US market by the FDA and from the UK market by NICE. This mesh is still used in other countries so if your surgeon is recommending this procedure, you should seek a second opinion.
The procedure itself involves stitching mesh into the top of the vaginal fault if there is no uterus present, or into the top portion of the vagina and surrounding the cervix if the uterus is still in place. The mesh is stitched both on the front and back side of the vagina in both cases. The opposite end of the mesh is then stapled (with titanium stables) into your sacrum bone. As well as the common adverse reactions from mesh (including erosion, pain etc.) this particular procedure has resulted in some extremely unusual complications. The image illustrates the Sacrocolpopexy (no uterus). Removal of this type of mesh is complicated and generally requires obliterative surgery.
Some Final Words on Synthetic Mesh Grafts
In a 60 minutes documentary a leading plastics expert explained that polypropylene should not be permanently implanted in the human body. Mesh devices are PERMANENT. Pelvic organ prolapse mesh can reach all the way from the front to the back of the pelvis in some cases, and is both difficult and dangerous to remove. Those who suffer complications can end up with repeated surgeries to have portions of the mesh snipped away, creating further damage and not necessarily resolving the issues. Even removal doesn’t guarantee a return to normal.
This is a global issue. You can watch documentaries from The Bleeding Edge on Netflix, Sky News in UK, W5 in Canada and ABC News in Australia. Similar mesh is used for hernia operations which is also causing serious health issues according to this BBC documentary released in 2017. The decision to implant synthetic mesh is not one to be taken lightly, so consider your options carefully
Conservative Treatment for Pelvic Organ Prolapse
Having viewed the invasive (surgical) treatments for Pelvic Organ Prolapse, you may also be interested in the conservative (non-surgical), which you can get to from the button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
Explore the Other Types of Pelvic Organ Prolapse
You may be interested in exploring the other types of prolapse. You can do that from here:
References
- Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997 Apr;89(4):501-6. doi: 10.1016/S0029-7844(97)00058-6. PMID: 9083302.
- Milani, A.L., Damoiseaux, A., IntHout, J. et al. Long-term outcome of vaginal mesh or native tissue in recurrent prolapse: a randomized controlled trial. Int Urogynecol J 29, 847–858 (2018). https://doi.org/10.1007/s00192-017-3512-3.
- Maher C, Feiner B, Baessler K, Christmann‐Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database of Systematic Reviews 2016, Issue 11. Art. No.: CD004014. DOI: 10.1002/14651858.CD004014.pub6. Accessed 28 November 2021.
- Schiavi MC, Perniola G, Di Donato V, Visentin VS, Vena F, Di Pinto A, Zullo MA, Monti M, Benedetti Panici P. Severe pelvic organ prolapse treated by vaginal native tissue repair: long-term analysis of outcomes in 146 patients. Arch Gynecol Obstet. 2017 Apr;295(4):917-922. doi: 10.1007/s00404-017-4307-y. Epub 2017 Feb 21. PMID: 28224269.
- Dällenbach P. To mesh or not to mesh: a review of pelvic organ reconstructive surgery. Int J Womens Health. 2015 Apr 1;7:331-43. doi: 10.2147/IJWH.S71236. PMID: 25848324; PMCID: PMC4386830.