POP-Q Measurement System for Prolapse
What Is the Pop-Q Measuring System?
In 1996, as transvaginal mesh slings were being introduced to the market, a committee from the International Continence Society (ICS), in collaboration with the American Urogynecology Society (AUGS) were tasked with creating a standard system of terminology to effectively describe pelvic organ prolapse in women. The “POP-Q” system, as well as providing standard terminology, provided a way to quantify and measure the level of pelvic organ prolapse. As with any “standard system”, it was intended to identify “normal” and to find a uniform way to specify the different stages of prolapse. This should ensure that specialists, regardless of where they are in the world, can speak the same language regarding pelvic organ prolapse (rectocele, enterocele, cystocele and uterine prolapse). The diagram below shows the POP-Q system parameters.
Pop-Q Measuring for Prolapse
| Aa | Center of Front Vaginal Wall |
| Ba | Highest Point Vaginal Wall (Front) |
| C | Bottom Edge of Cervix |
| D | Highest Point in Vagina |
| Ap | Center of Back Vaginal Wall |
| Bp | Highest Point Vaginal Wall (Back) |
| tvl | Total Vaginal Length |
| gh | Genital Hiatus |
| pb | Perineal Body |
The POP-Q markings may look complicated but the method is actually quite simple. Let’s start with gh (genital hiatus) which is the space between the vaginal opening and the vagina as shown in the external view.
The hiatus is actually an opening in your puborectalis muscle (part of your levator ani muscle of the pelvic floor). When the size of this opening is increased, it indicates laxity of the pelvic floor which is one of the underlying causes of pelvic organ prolapse. If this gap is larger than expected, pelvic floor muscle training (PFMT) will be needed.
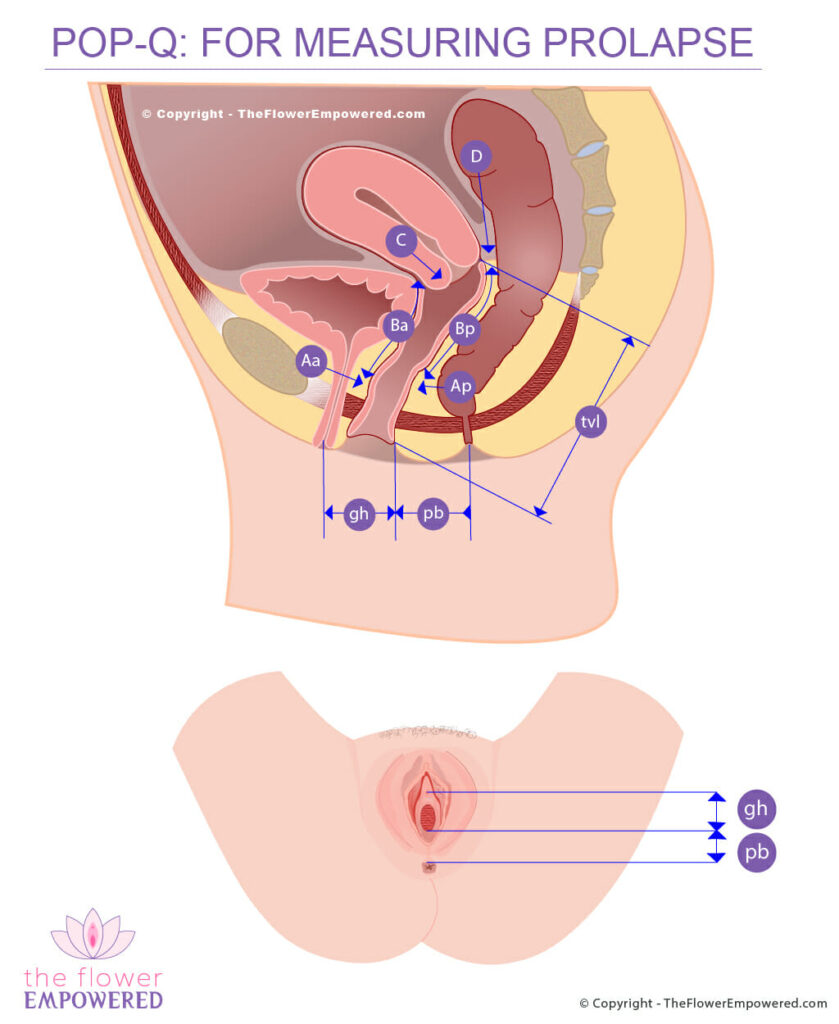
Next we can look at the pb (perineal body). Did you know there are three layers of muscles that make up your pelvic floor? The perineal body is an intersection for many of the muscles within these layers and plays an important role in the functional stability of your pelvic floor. During vaginal birth, the perineum often tears or is sometimes cut with scissors (episiotomy). Oftentimes, the job of stitching up the perineum after birth is not adequate leaving instability (which also results in a larger genital hiatus). By measuring this area, your doctor gains valuable information about the condition of your perineal muscles and the tone of your pelvic floor. PFMT will help a lot with restoring strength and bulk to this area.
Total vaginal length (tvl) is exactly that – the length of your vagina from the just inside the vaginal opening (hymen) to the very deepest point. With prolapse, your organs can fall out of your vagina, so knowing its length allows doctors to see the depth of your prolapse. Once everything is back in place, doctors can also measure the result of the anatomical repair.
Aa and Ap are the mid point of the front (anterior) and back (posterior) walls of the vagina respectively. For the purpose of uniformity, in a normal vagina with no prolapse, this point is assumed to be 3cm up from the hymen just inside the vaginal opening. Measurements range from -3 (no prolapse) to +3 (prolapsed completely past the hymen)
Ba and Bp are the highest points in the vagina for the front wall (anterior) and back wall (posterior). As both Ba and Bp are measured from point Aa and Ap, they are assumed to be -3 for a normal vagina with no prolapse. For each cm these points descend, a cm is added to this measurement up to total vaginal length if the entire vagina is prolapsed.
Point C measures the edge of the cervix. This measurement is used to see if the cervix is prolapsing. Point D is then compared to Point C to gauge if the opening to the cervix has been stretched.
Treatment for Pelvic Organ Prolapse
Like most symptoms of pelvic floor dysfunction, the treatment for Pelvic Organ Prolapse falls into one of two categories; conservative (non-surgical) and invasive (surgical). Surgical options are generally only advised for severe prolapse (grade 3 or 4). For more information on the various treatments offered in these two categories, click on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
Explore the Different Types of Pelvic Organ Prolapse
You may be interested in exploring the other types of prolapse. You can do that from here: