Women With Pelvic Floor Dysfunction Have Decreased Quality of Life1
What Is Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction is a condition where you cannot properly contract or relax your pelvic floor muscles. On this page you will learn about your pelvic floor muscles and what happens when they become dysfunctional. You will also learn about pelvic floor muscle training (PFMT) which is the primary treatment for pelvic floor dysfunction2. We have many additional pages that explain the different symptoms and treatments for the various conditions that are caused by pelvic floor dysfunction. If you don’t find the information you are looking for, we have a search bar at the bottom of the page that will search the site including all pages and articles. You can also jump onto our community and ask questions there. As always, speak to your doctor or another healthcare professional if you believe you may have pelvic floor dysfunction.
What Do Your Pelvic Floor Muscles Do?
Your pelvic floor muscles provide a platform beneath your pelvic organs. It is called your pelvic “floor” because it acts like an elastic floor covering the base of your pelvis. It’s a floor with a number of openings to the outside world; Firstly, the urethral opening through which you pee. Secondly the vaginal opening which is the opening through which your period flows and your baby is delivered. Lastly the rectal opening through which you poop.
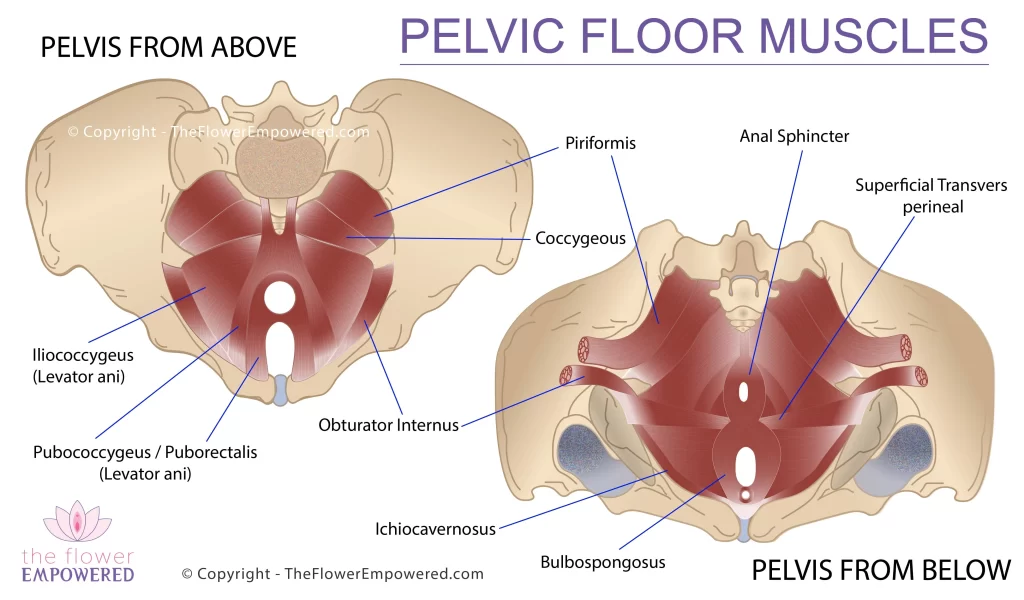
Pelvic Floor Muscles
Your pelvic floor is made of three different layers of muscle which work together to maintain urinary and fecal continence. Your pelvic floor muscles are also involved in sexual function. The image shows your pelvic floor muscles within the pelvis from above and below.
Just like the muscles elsewhere in your body, if you don’t use them or you injure them, they can become weak and may not function effectively. A well functioning pelvic floor will have a resting length that allows it to both contract and relax when needed.
If you would like more detail on the individual muscles and their function, their workings are explained in detail in the book, Empower Your Flower.
What Is a Hypertonic or Hypotonic Pelvic Floor?
If you pelvic floor is hypertonic (tight), that means that it’s resting length is shortened. This does not mean that your pelvic floor is stronger than normal as a shortened muscle cannot contract further. A dysfunctional pelvic floor that is hypertonic is typically referred to as having Non-Relaxing Pelvic Floor Dysfunction (NR-PFD)3. A hypertonic pelvic floor will typically sit higher than a normally functioning pelvic floor.
Hypertonic pelvic floor muscles can cause symptoms such as overactive bladder, urinary retention, pelvic pain, constipation, vaginismus, dyspareunia. Hypertonic pelvic floor muscles can make it feel like there is something in your vagina, similar to the symptoms of prolapse. It is important to get your pelvic floor checked by a healthcare professional to rule out hypertonicity if you have any of these symptoms.
If you pelvic floor is hypotonic (weak), that means that it’s resting length is lengthened. This can be due to muscle atrophy, where there is loss or thinning of your muscle tissues. Muscle atrophy can be caused by lack of use or ageing. A dysfunctional pelvic floor that is hypotonic is typically referred to as having Pelvic Floor Dysfunction (PFD). A hypotonic pelvic floor will typically sit lower than a normally functioning pelvic floor.
Hypotonic pelvic floor muscles can cause symptoms such as stress incontinence, mixed incontinence, pelvic organ prolapse, constipation and sexual dysfunction. With a hypotonic pelvic floor, there can be loss of sensation making it more difficult to contract the muscles. You should have your pelvic floor checked by a pelvic floor physical therapist if you believe you have hypertonic pelvic floor muscles.
The pelvis to the left shows how a hypertonic pelvic floor, which sits higher, creates more compression around the openings of the pelvic floor. Hypertonic pelvic floor muscles make it harder to relax the pelvic floor. The pelvis in the center shows how a normally functioning pelvic floor sits in a balance position and can contract or relax easily. The pelvis to the right shows how a hypotonic pelvic floor sits lower and creates less compression around the pelvic organs. Hypotonic pelvic floor muscles make it harder to contract the pelvic floor.
Treatment for Pelvic Floor Dysfunction
If you are diagnosed with Pelvic Floor Dysfunction, you should make an appointment with a Pelvic Floor Physical Therapist (Physiotherapist) for an assessment. They will check if you have hypertonicity or hypotonicity, which has a bearing on your treatment options. The primary treatment for pelvic floor dysfunction is pelvic floor muscle training (PFMT).
In the case of pelvic floor hypertonicity (tight), this training involves pelvic floor relaxation exercises (reverse Kegels). For pelvic floor hypotonicity (weak), the training involves pelvic floor strengthening exercises (Kegels). Studies have shown that pelvic floor muscle training significantly improves the quality of life in women with urinary incontinence4. Our YouTube channel shares many videos for both pelvic floor relaxation and pelvic floor strengthening. You will see two examples below.
Kegels for Pelvic Floor Relaxation
Kegels for Pelvic Floor Strengthening
Is Pelvic Floor Muscle Training the Only Treatment?
You may be wondering if pelvic floor muscle training is the only treatment for pelvic floor dysfunction and the answer is no. The treatment options are very much dependent on the symptoms that are present. Pelvic floor dysfunction can impact urination, defecation and sexual function. It is more complex than simply changing the balance of tension within the pelvic floor (although that does go a long way towards overcoming the symptoms). In this knowledge portal, we have pages explaining each of the different symptoms along with their treatment options, both conservative and surgical. You can use the button links below to jump to that symptom’s page or use the search bar at the bottom of the page to help you find what you are looking for.
Information on Specific Symptoms and Treatments
Symptoms of Hypertonicity
Symptoms of Hypotonicity
References
- Segedi LM, Ilić KP, Curcić A, Visnjevac N. [Quality of life in women with pelvic floor dysfunction]. Vojnosanit Pregl. 2011 Nov;68(11):940-7. Serbian. doi: 10.2298/vsp1111940m. PMID: 22191311.
- Hay-Smith EJ, Dumoulin C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2006 Jan 25;(1):CD005654. doi: 10.1002/14651858.CD005654. Update in: Cochrane Database Syst Rev. 2010;(1):CD005654. PMID: 16437536.
- Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clin Proc. 2012 Feb;87(2):187-93. doi: 10.1016/j.mayocp.2011.09.004. PMID: 22305030; PMCID: PMC3498251.
- Radzimińska A, Strączyńska A, Weber-Rajek M, Styczyńska H, Strojek K, Piekorz Z. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: a systematic literature review. Clin Interv Aging. 2018 May 17;13:957-965. doi: 10.2147/CIA.S160057. PMID: 29844662; PMCID: PMC5962309.