Pelvic Floor Muscle Training Is Effective in Conservative Management, Especially in Women With Mild to Moderate Prolapse(Stages 1-3)1
Conservative Treatments for Pelvic Organ Prolapse
When it comes to non-surgical treatments for pelvic organ prolapse, the options depend largely on the stage to which the prolapse has progressed. You don’t develop a stage 4 pelvic organ prolapse overnight. It can take years for the herniation to progress to a late stage prolapse, so it really makes sense to work on maintaining a healthy pelvic floor while managing your intraabdominal pressures (that’s right, no straining ladies!). The most basic conservative treatment for pelvic organ prolapse is pelvic floor muscle training (PFMT).
If you have a good relationship with your lady-parts, and you maintain the strength of your pelvic floor, your chances of developing a stage 3 or 4 prolapse are greatly diminished. If you have not noticed your pelvic organ prolapse until your organs have started to protrude outside of your vaginal opening, you may require a surgical repair. Regardless of whether or not surgery is needed, PFMT is always required. To have surgery without undertaking rehabilitation of your pelvic floor muscles is the equivalent to treating the symptom without addressing the root cause. Training your muscles also trains your connective tissue by encouraging fibroblasts to create new fibres in the supporting structures based on the pattern of your movements.
Pelvic Floor Muscle Training (PFMT)
Traditional pelvic floor muscle training is the primary non-surgical treatments for pelvic organ prolapse. PFMT involves exercising pelvic floor muscles to restore muscle strength and function. These exercises are often called Kegels – named after Dr. Arnold Kegel who first identified the importance of strengthening these muscles to maintain a stable vaginal canal. It is important to learn how to perform Kegels properly. Strengthening the pelvic floor will help to “lift” your floor in order to provide better support of your pelvic floor organs, while giving your fascia the opportunity to readjust.
Consistency and variation with is key. By performing the exercisers in varying positions and consistently practicing daily, you should see improvement, even when there is substantial weakness to begin with. You can sign up for our 30 day challenge to get an insight into what varied training looks like. When you sign-up, you will get access to a bonus video that goes through the steps to perform a complete Kegel while also making a short self-assessment of your ability to contract your pelvic floor. This is not intended to replace a proper assessment by your healthcare professional.
Additional Conservative Treatments for Pelvic Organ Prolapse
Pelvic floor muscle training focuses solely on strengthening your pelvic floor muscles. However, your pelvic floor muscles do not work in isolation. Taking an approach that retrains the muscles that support the hips including the core, the glutes and muscles in throughout the rest of your body will improve your chances of optimising your pelvic health. Not only will all-body training help to improve strength and coordination, it should also help you to learn to balance intraabdominal pressure. The eight-phase training detailed in the book Empower Your Flower offers all-body training to help rebalance tension and improve coordination. In the next section, we will list five additional non-surgical treatments for pelvic organ prolapse.
1. Hypopressive Breathing Exercises
Hypopressive breathing exercises use stomach vacuums to lift the contents of the abdominopelvic cavities upwards, which can help to relieve the symptoms of prolapse. Studies have shown that pelvic floor muscle training is more effective at treating pelvic organ prolapse than hypopressives3. However, even though PFMT is superior, combining a hypopressive practice with pelvic floor muscle training can be of benefit. The eight-phase training includes both pelvic floor muscle training and hypopressive breathing exercises.
2. Weight Management
As your BMI increases, so too does your intra-abdominal pressure. An increase in intra-abdominal pressure directly increases the pressure on the pelvic floor. Over time, this added pressure can lead to weakness which in turn increases the risk of developing POP. A 2009 study found that “being overweight or obese is associated with progression of POP”. The same study found that weight loss does not appear to be significantly associated with regression of POP. They assumed that the damage to the pelvic floor from weight gain was irreversible. However, NONE of the participants in the study underwent PFMT. Studies into PFMT for clearly demonstrate that, not only does PFMT strengthen the pelvic floor, it also significantly improves the symptoms POP.
3. Improve Your Posture
Your posture and alignment can directly impact the stability of your pelvic floor and should be assessed as part of your rehabilitation. One study found that an abnormal change in spinal curvature, specifically, a loss of lumbar lordosis, appears to be a significant risk factor in the development of pelvic organ prolapse2. Your connective tissue is responsible for holding your shape, managing your posture and distributing load. If your posture is impacting your pelvic floor, you can work with a physical therapist or structural integrator to help bring you back into balance.
4. Quit Smoking
A 2005 study concluded that “tobacco smoking is an independent risk factor for pelvic organ prolapse”. Smoking contributes to a breakdown of vaginal elasticity which can contribute to weakness. If you smoke or spend substantial time passively smoking (in the presence of a smoker), you should consider making some changes to limit your exposure. You should also consider the impact of coughing on your pelvic floor. Coughing is increased with smoking. Each cough gives a sudden burst of intra-abdominal pressure, which over time, can negatively impact your pelvic floor.
5. Group Training
A randomised study evaluated the effects of pelvic floor muscle training between two groups. Group 1 did PFMT at home alone, while group 2 did PFMT at home combined with one group training session per week. Group 2 participants showed significant improvement in pelvic floor muscle function compared with group 1. This emphasises the importance of community and working together to achieve our goals. Physically meeting with other women all sharing a common goal helps you to stay accountable thus increasing your chances of success. There are many classes that focus on pelvic health. If your pelvic health physiotherapist does not offer a weekly group sessions, try to find a pilates, yoga or hypopressive class focusing specifically on pelvic floor training.
Pessaries for Pelvic Organ Prolapse
Pessaries are often used to help manage pelvic organ prolapse. They can be used temporarily or long term and often give immediate relief to symptoms. Although you can buy disposable pessaries online, they are only a short term solution. It is best to visit your pelvic floor physical therapist to get fitted for a reusable pessary. Finding the correct size and shape requires some experimentation, but your pelvic floor physical therapist is trained to and help you with fitting. You should not feel the pessary when it is in place (similar when you use a tampon). Pessaries, like tampons and menstrual cups, do come with the risk of developing toxic shock syndrome. Although this is rare, you should still be aware of the signs.
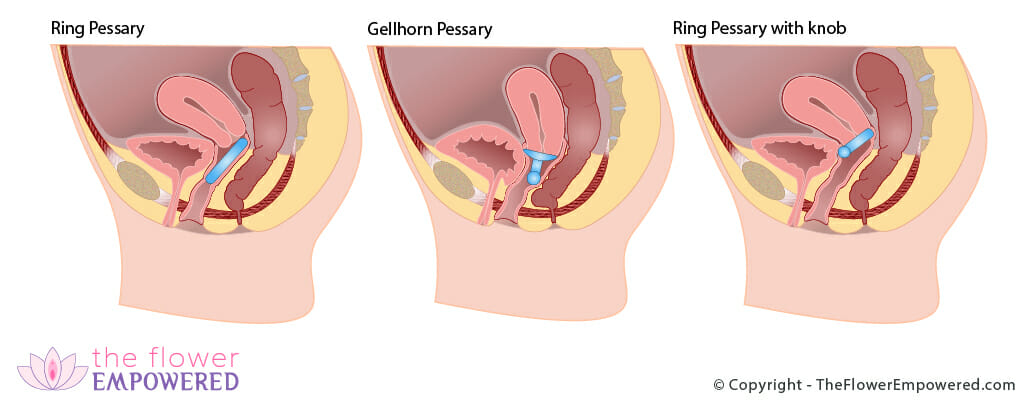
There are two different types of pessary; supportive and space filling. Supportive pessaries, such as ring pessaries, can be worn during intercourse. Space filling pessaries need to be removed before intercourse. The image below shows some a few different types of pessaries.
Measuring Your Progress
You cannot manage what you do not measure, so before beginning any program of rehabilitation, should begin with establishing your baseline. This allows you to properly assess your progress. There are multiple ways to measure your progress. Biofeedback is one of the most consistent ways to measure your pelvic floor muscle strength, as a biofeedback device will actually measure the strength of your contractions. If you go to see a pelvic floor physical therapist, they can perform biofeedback or ultrasound to directly see the activation of the pelvic floor. They will also track your POP-Q scores which will help to show your progress. Dramatic improvement in symptoms is typically experienced with only slight improvements to POP-Q scores. Change in the body takes time and consistency. Be patient with yourself.
Products for Management of Pelvic Organ Prolapse
There are many products that can be used in the management pelvic organ prolapse. We have include some of those products below. You should speak with your pelvic floor physiotherapist or doctor before using these products. Reviews of these products will be covered on our YouTube channel. If there is a specific product that you would like to see reviewed, just get in touch and we will review. Note that these products have affiliate links. Should you choose to purchase them, we will make a small commission.
Rectocele Splinting Aid
Innovo E-Stim Shorts
New Non-Surgical Pelvic Organ Prolapse Treatment Based on the Latest Research
The most exciting new treatment for pelvic organ prolapse takes a biotensegrity approach utilising a myofascial release technique to restore pelvic organs to their normal anatomical position. The initial retrospective study used postural assessment, pelvic tissue examination, and myofascial release of taut pelvic tissue, trigger points, and scar tissue. Many of the participants in the study had more than one type of prolapse (some having up to four different prolapses simultaneously). All women reported an improvement in prolapse symptoms. Further studies are underway, meanwhile, this study highlights the benefits of pelvic floor relaxation when working to overcome pelvic organ prolapse.
Explore the Invasive Treatments for Pelvic Organ Prolapse
Having reviewed the non-surgical treatments for Pelvic Organ Prolapse, you may be interested in the surgical options. You can do that from here:
Explore the Other Types of Pelvic Organ Prolapse
You may be interested in exploring the other types of prolapse. You can do that from here:
References
- Basnet R. Impact of pelvic floor muscle training in pelvic organ prolapse. Int Urogynecol J. 2021 Jun;32(6):1351-1360. doi: 10.1007/s00192-020-04613-w. Epub 2021 Jan 8. PMID: 33416965.
- Mattox TF, Lucente V, McIntyre P, Miklos JR, Tomezsko J. Abnormal spinal curvature and its relationship to pelvic organ prolapse. Am J Obstet Gynecol. 2000 Dec;183(6):1381-4; discussion 1384. doi: 10.1067/mob.2000.111489. PMID: 11120500.
- Resende APM, Bernardes BT, Stüpp L, Oliveira E, Castro RA, Girão MJBC, Sartori MGF. Pelvic floor muscle training is better than hypopressive exercises in pelvic organ prolapse treatment: An assessor-blinded randomized controlled trial. Neurourol Urodyn. 2019 Jan;38(1):171-179. doi: 10.1002/nau.23819. Epub 2018 Oct 12. PMID: 30311680.