When All Invasive Treatment Options Are Transparently Presented to Female Patients With SUI, They Prefer Other Surgical Treatments as an Alternative to MUS.1
Invasive Treatments for Urinary Incontinence
When it comes to surgical treatments for urinary incontinence, there are a number of alternatives available and the options presented to you will be dependent on your specific symptoms. Some of the treatments can be considered minimally invasive involving injections, while others are surgical. The surgical options will be dependent on your surgeon’s experience and preferences.
Graft or Native Tissue for Stress Incontinence
One of the key decisions to be taken when performing surgical treatment for stress incontinence is whether or not to use a graft material (mesh) or native tissue during the repair. A 2021 study into the long term safety with mesh slings implanted in 36,195 women found that “1 in 27 women had sling erosions and 1 in 15 had invasive reoperations at 7 years after sling procedures“2. Many countries have removed mesh devices from the market while others are urging extreme caution when using mesh implants. Patient support groups are working diligently to ban the use of mesh products completely.
On this page, we will present minimally invasive options before presenting the surgical options, which we will separate into lower risk non-mesh surgeries and the higher-risk mesh surgeries. You need to remember that all surgeries carry risks, even those considered to be “minimally invasive” using native tissue. Carefully consider your options and make sure to get a second opinion if you are unsure.
Important Considerations Before Undergoing Surgery
It is important to note that all surgeries carry risks and none have a 100% success rate. Surgery in the pelvic area has the potential to damage organs (bladder, uterus, bowel) as well as nerves, blood vessels and muscle/fascia.
Following incontinence repairs, you could experience symptoms that you did not have prior to your surgery, such as de novo incontinence (incontinence you did not have prior to surgery) or overactive bladder (OAB). You may also experience Pelvic pain and sexual dysfunction.
You should consider dedicating at least 18 months to conservative options before undertaking any surgery. Surgical repair will not make your pelvic floor stronger or more relaxed. There is no such thing as a quick-fix for stress incontinence or overactive bladder. Following any pelvic floor surgery, you should work with your pelvic floor physical therapist to rehabilitate your pelvic which can help to mitigate any new symptoms.
Set Appropriate Expectations Before Surgery
It is important to have realistic expectations if you are having surgery, and to ensure that your surgeon is aware of your expectations. What you believe to be surgical success might not be the same as your surgeons view of success. Studies into the surgical treatment of incontinence typically measure success either as object cure rate, subjective cure rate or a combination of the two. Within a single study, the objective and subjective cure rates can vary greatly. A good example of this is this study from 2012 comparing two different mid-urethral slings for the treatment of SUI. For TVT mesh sling, the subjective cure rate was 79,8% whereas the objective cure rate was 95%. For TVT-O mesh sling, the objective cure rate was 95% but the subjective cure rate was 54,8%. How is this possible?
Let’s use a simple example: A patient has surgery for SUI where a mesh device is implanted. Following surgery, the symptoms of stress incontinence have disappeared, therefore she is objectively cured. However, she now suffers pain during intercourse and is no longer able to have sex. Although her incontinence has been cured, she views this surgery as unsuccessful due to the impact on her quality of life.
A Shortened 6-Week Treatment Protocol With PTNS Appears to Be Successful and More Effective Than Sham in the Treatment of Refractory OAB.3
Minimally Invasive Options for Urinary Incontinence
There are multiple minimally invasive options available to treat the different types of incontinence. Your doctor or surgeon can help to decide which option could be best for you. Some of these treatment options are detailed below.
Urethral Bulking for Stress Incontinence
You may be familiar with lip fillers that are used to bulk the lips in order to exaggerate their size pout. A similar treatment is available to add bulk to the tissues surrounding the urethra. Fillers break down over time as the body disposes of the product that has been injected. As such, the results achieved by fillers are short term. This means that repeat treatment is subsequently required in order to reproduce the initial results.
Some of the side effects include urinary tract infection, urinary retention, de novo urgency, migration into lymph nodes and erosion4.
Urethral Bulking
PTNS for Overactive Bladder
Posterior Tibial Nerve Stimulation (PTNS) is the more invasive version of tibial nerve stimulation (which is shown on the non-surgical treatments page). Instead of using two skin electrodes, one of the skin electrodes is replaced with a needle which is inserted into the inner ankle.
You sit in a chair with your legs elevated. The needle is inserted about the width of three fingers above the malleolus (ankle bone). The skin electrode is placed under the foot in the calcaneus. It is normal for the big toe to flex during treatment. Some studies say you should feel the contraction of your pelvic floor during treatment, although this is not always felt.
Posterior Tibial Nerve Stimulation (PTNS)
Laser Treatments for Stress Incontinence
Laser treatments have been used for many years to treat skin conditions. There are a number of laser treatments being offered to treat stress urinary incontinence. Originally, laser vaginal treatment was used in plastic surgery with terms like “rejuvenation” and “vaginal tightening” being used to market the treatments. This caused some medical professionals to raise concerns as to whether these procedures were ethical. A 2015 study showed some promising, with 77% of patients with SUI showing improvement at one year follow-up.
Laser Treatment
Botox Injection for Overactive Bladder
If you are familiar with the use of botox to relax the muscles of the forehead, you will easily understand this treatment. Botox is injected into the bladder to reduce the contractions of the bladder muscle (detrusor). This treatment, like that of the forehead, is only a short term measure, typically lasting for several months before a repeat procedure is required. Unfortunately, the two main side effects are urine retention and urinary tract infection which happens in 10% and 20% of patients respectively. If all of the more conservative options have failed, your urologist may want to try botox as your next treatment.
The treatment is performed by inserting a cystoscope through a small tube into the urethra. The bladder is filled with sterile water. The detrusor muscle is then injected with many very small injections. It typically takes 5 to 10 minutes for this treatment to be completed.
Botox Injection Into the Bladder
The Autologous Pubovaginal Sling Procedure for the Treatment of Stress Urinary Incontinence Offers the Highest Success Rate and Is the Most Commonly Used PVS Surgical Method5
Non-Mesh Urinary Incontinence Surgical Treatments
In this section, we will review the non-mesh surgical treatments for urinary incontinence. There are two main non-mesh surgeries offered to treat SUI: retropubic suspension, which involves supporting the urethra with sutures, and sling surgery, which involves supporting the urethra with a biological graft. Biological grafts can be autologous (fascia/connective tissue taken from your own body), Allograft (fascia/connective tissue taken from a cadaver) or Xenograft (animal derived collagen tissues typically from a cow or pig).
Although the surgeries in this section are primarily focused towards stress incontinence, they are also sometimes offered to patients who have OAB without the presence of stress incontinence. Following the explanation of these non-mesh and mesh surgeries for incontinence, we will review the SNS surgical procedure for OAB.
Retropubic Suspension (Urethropexy)
Retropubic Suspension (Urethropexy) is a procedure where sutures are used to improve the positioning of the urethra to prevent stress incontinence. The surgery treats stress incontinence by lifting the neck of the bladder using sutures. It was first performed in 1962 by Dr. John Burch.
There have been several modifications to the technique over the years such as the Marshall-Marchetti-Krantz (MMK). These procedures are performed either as open or keyhole (laparoscopic) surgery. The main difference between the Burch and MMK is the placement of sutures on the pubic side, with Burch sutures are attached to Coopers Ligament. With MMK sutures are attached to the periosteum of the pubic symphysis. You can see an example of these procedures in the images below.
The surgery is performed by making a small incision in your lower abdomen, just above your pubic bone, and placing the sutures. There have been many long term studies into these procedures and success of the Burch procedure is reported to be 90% with 5 to 10 year follow-up and 69% with 10 to 20 year follow-up. The MMK on the other hand has shown lower-success long term. Retropubic suspension is considered to be the gold standard for stress incontinence when there is urethral hyper-mobility.
Autologous Pubovaginal Sling (PVS)
Biological slings were the first ever slings used to treat SUI back in 1907 when Giordiano used the gracilis (a muscle from the inner thigh) to support the bladder neck. Over subsequent years, other muscles were used until eventually, it was realised that muscles were not ideal graft material due to difficulty with maintaining good blood and nerve supply.
The focus turned to using fascia, harvested either from the rectus abdominis (lower abs) or the fascia lata (large band of fascia down the outside of leg). The first major study to confirm that autologous facial slings were safe and effective was in 1978 by McGuire et al.
The native biological sling, also known as Autologous Pubovaginal Sling (PVS) is attached to the rectus fascia above the pubic bone and runs under the urethra providing additional support. Surgery itself involves taking the graft of the connective tissue just below your abs or alternatively taking a graft from your Fascia Lata which runs down the outside of your thigh.
The graft is soaked in an antibiotic solution before implantation. You will have an incision in your lower abdomen just above the pubic bone and one just inside the vagina. Surgery should last about an hour and has a recovery time around six weeks. With this type of surgery, you can expect to be in hospital overnight. According to the British Association of Urological Surgeons (BAUS), success rates for PVS are the same as with mid-urethral sling (mesh) procedures.
Allograft slings (from cadaver) and xenograft slings (from an animal) were introduced around the same time as synthetic mesh, however, they didn’t receive the same level of uptake. A study in 2014 found that the costs of repair with synthetic mesh were roughly a quarter of that of biologic mesh. Mesh manufacturers make payments to doctors, hospitals and medical societies that make it even more profitable to use synthetic mesh. Some of the information on payments is now available on dollars for docs and on the open payments data websites.
The concludes the surgical treatments with native tissue. We will now explore the options using mesh grafts.
A 2021 Systematic Review, Found Compelling Evidence That MUS Complications Remain Under-Reported in the Literature and Are Higher Than Previously Thought6
Mesh Graft Surgical Treatments for SUI
In this section, we will review the surgical treatments for incontinence using synthetic mesh grafts. If you are offered a surgical repair using any graft that is not your own native tissue, you should be aware that those graft materials come with higher risks. The benefit of using these grafts does not generally outweigh these risks.
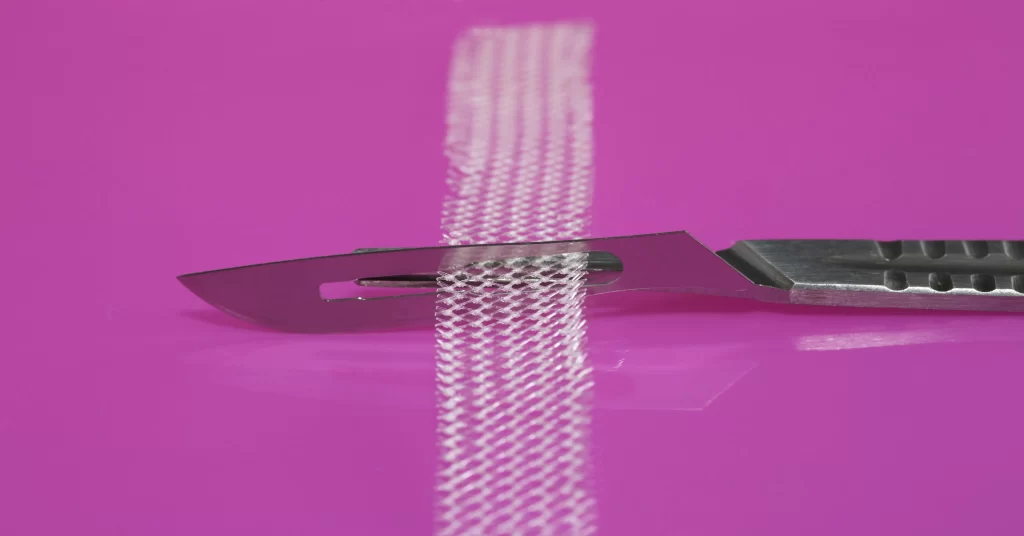
Synthetic meshes are typically made with polypropylene (also called prolene) which is the same material used to make the blue IKEA bags. When doctors talk about mesh slings, they can call them by many names – tape, ribbon, elastic band etc. They can also refer to them as mid-urethral slings (MUS). These MUS’s fall into three categories – TVT, TVT-O and mini-slings (also known as single incision slings – SIS). Regardless of what they are called, they are made from a knitted synthetic plastic. We will review the different mesh grafts in this section.
Mid Urethral Sling (MUS) – Transvaginal Tape (TVT)
Mid-urethral synthetic slings have been in use since the mid 90’s. The TVT (Trans-Vaginal Tape) is a retropubic mesh sling. It can be implanted “bottom up” or “top down”. For top down, it is implanted by first making three small incisions, two just above the pubic bone on the left and right side, and one inside the vagina in front of the urethra.
The sling is attached to two large needles (known as trochars). The needles are blindly inserted into the vagina and guided past the bladder, blood vessels and nerves, eventually emerging through the small holes above the pubic bone.The blind insertion increases the risk of bladder perforation.The tape lies flat against the urethra and is checked to ensure there is no tension. For this reason, it is also known as “tension free vaginal tape”. The incisions are then closed.
Bottom-up implantation involves the same incisions but the needles are blindly fed through the hole in the vagina finally exiting in the incisions above the pubic bone. In some cases, a small camera may be used to help guide the needles. Bottom-up implantation is the preferred route with some studies suggesting a lower number of bladder perforations with this approach than with a top-down approach.
There are several manufactures of mesh for POP repairs, the main ones being; J&J Ethicon, Boston Scientific, American Medical Systems, Bard and Coloplast.
MUS – TVT Obturator (TVT-O) – Trans-obturator Tape (TOT)
The TVT-O (Trans-Vaginal Tape – obturator) and TOT (Trans obturator tape) involve placing a mesh sling in the space between the left and right obturator foramen. TVT-O is implanted inside-out with TOT is implanted outside-in.
For TVT-O, an incision is made inside the vagina in front of the urethra. The sling is attached to two large needles (known as trochars). With the inside-out approach, the first needle is inserted into the vagina and guided past muscles, blood vessels and nerves until the fascia at the obturator membrane is perforated.
The curved needle is then rotated towards a small mark the surgeon has made on the inside of the patients leg close to the groin. The needle is pushed through the obturator externus muscle, two of the adductor muscles (Magnus & Brevis) and the gracilis muscle before coming through the skin. This is repeated on the other side.
For TOT with the outside-in approach, two incisions are made on the inside of the legs close to the groin and one in the front wall of the vagina. The needle is fed in through the groin on one side, going through the same muscles and past the nerves, blood vessels and connective tissue as with the inside out approach. once the needle makes it to the hole in the vaginal wall, the needle is then guided up through the tissues to come out at the groin incision on the opposite side.
With both approaches, the tape lies flat against the urethra and is checked to ensure there is no tension. The incisions are closed following implantation. Most studies show little difference between efficacy with the two different approaches. As well as mesh erosion, infection and vaginal pain, patients with this type of mesh sling often suffer from leg pain and can have difficulty walking.
MUS – Single Incision Sling (SIS)
he Single Incision Sling (SIS) also know as the mini-sling is a TVT-O/TOT type mesh sling, however, unlike the TVT-O/TOT, the mini-sling attaches to the obturator membrane. This type of sling requires only a single incision in the vagina beneath the urethra. The first of these devices to be introduced to the market was the TVT-Secur (also known as the TVT-S). That device is no-longer on the market due to the sheer volume of issues it created with some studies concluding it was inferior to TVT and TVT-O. Other mini-slings and single incision slings (SIS) are still on the market but cannot be viewed as safe as none have been through proper testing, instead being given approvals based on predecessors, the most studied of which is the TVT-Secur.
Like the TOT, the SIS mini-sling application needle is inserted through an incision in the vagina just behind the urethra. The needle is guided past muscles, blood vessels and nerves. Depending on the specific sling (there are multiple brands), it will either be guided to the obturator muscle or into the obturator membrane. The mesh is placed flat against the urethra with no tension. There are no additional incisions required with this surgery. Mini-slings and SIS devices need some form of adhesion to ensure they attach and stay in place. Some have an adhesive surface, while others have anchors or barbs that have some abrasion allowing them to grip the muscle or connective tissue to which they will attach.
Some Final Words on Synthetic Mesh Grafts
In a 60 minutes documentary a leading plastics expert explained that polypropylene should not be permanently implanted in the human body. Mesh devices are PERMANENT. Pelvic organ prolapse mesh can reach all the way from the front to the back of the pelvis in some cases, and is both difficult and dangerous to remove. Those who suffer complications can end up with repeated surgeries to have portions of the mesh snipped away, creating further damage and not necessarily resolving the issues. Even removal doesn’t guarantee a return to normal.
This is a global issue. You can watch documentaries from The Bleeding Edge on Netflix, Sky News in UK, W5 in Canada and ABC News in Australia. Similar mesh is used for hernia operations which is also causing serious health issues according to this BBC documentary released in 2017. The decision to implant synthetic mesh is not one to be taken lightly, so consider your options carefully
Sacral Nerve Stimulation (SNS) For the Treatment of OAB
Sacral Nerve Stimulation (SNS) is the most invasive treatment available for OAB. It involves implanting a pacemaker type device under the skin of the buttocks with an electrode that is fed into the S3 sacral nerve root.
This electrode produces a mild stimulation that helps to keep the bladder relaxed. The exact mechanism that makes this an effective treatment is not understood. It is hypothesised that the treatment is effective due to its stimulation of the S3 nerve root which contains sensory fibres for the pelvic floor and parasympathetic fibres connected to the detrusor (bladder muscle). SNS is not effective for all forms of OAB and tends to be more effective when urge incontinence is present than for OAB without incontinence.
The device is 2 inches wide and quarter inch thick. Battery life is expected to last 5 years, however, the device manufacturer emphasises that the more you use it, the quicker it will run out. Surgery is required to change the battery. You can do a two week trial before having the device implanted. During this trial period, you will have probes into your sacral nerve, having a small device strapped to your waist instead of being implanted.
Short and long term efficacy is reported to be good with some studies showing the success rate higher than less invasive methods. One study found that patients below 55 tended to have higher cure rates (65%) in comparison to older patients (37%). However, the rate of complication following surgery is in the 30-40% range within the first 5 years. Complications typically require re-operation (either for repair or removal) so decision to use this type of device should not be taken lightly. Unlike pelvic mesh devices, this device is not a permanent implant.
Conservative Treatment for Urinary Incontinence
Having viewed the invasive (surgical) treatments for Urinary Incontinence, you may also be interested in the conservative (non-surgical), which you can get to from the button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
Explore the Other Types of Urinary Incontinence
You may be interested in exploring the the different types of urinary incontinence. You can do that from here:
References
- Wyndaele M, Madhu C, Hashim H. Female stress urinary incontinence surgery: ‘Resurgence of the Titans’. Turk J Urol. 2021 May;47(3):210–5. doi: 10.5152/tud.2021.21073. Epub 2021 May 1. PMCID: PMC8260089.
- Chughtai B, Mao J, Matheny ME, Mauer E, Banerjee S, Sedrakyan A. Long-Term Safety with Sling Mesh Implants for Stress Incontinence. J Urol. 2021 Jan;205(1):183-190. doi: 10.1097/JU.0000000000001312. Epub 2020 Aug 4. PMID: 32749936.
- Lashin AM, Eltabey NA, Wadie BS. Percutaneous tibial nerve stimulation versus sham efficacy in the treatment of refractory overactive bladder: outcomes following a shortened 6-week protocol, a prospective randomized controlled trial. Int Urol Nephrol. 2021 Dec;53(12):2459-2467. doi: 10.1007/s11255-021-02999-0. Epub 2021 Oct 3. PMID: 34601705.
- Hoe V, Haller B, Yao HH, O’Connell HE. Urethral bulking agents for the treatment of stress urinary incontinence in women: A systematic review. Neurourol Urodyn. 2021 Aug;40(6):1349-1388. doi: 10.1002/nau.24696. Epub 2021 May 20. PMID: 34015151.
- Bayrak Ö, Osborn D, Reynolds WS, Dmochowski RR. Pubovaginal sling materials and their outcomes. Turk J Urol. 2014 Dec;40(4):233-9. doi: 10.5152/tud.2014.57778. PMID: 26328184; PMCID: PMC4548367.
- Lin YH, Lee CK, Chang SD, Chien PC, Hsu YY, Tseng LH. Focusing on long-term complications of mid-urethral slings among women with stress urinary incontinence as a patient safety improvement measure: A protocol for systematic review and meta-analysis. Medicine (Baltimore). 2021 Jun 18;100(24):e26257. doi: 10.1097/MD.0000000000026257. PMID: 34128853; PMCID: PMC8213295.