Surgery Is Necessary in a Very Small Fraction, Perhaps < 5% Of Patients1
Invasive Treatments for Fecal Incontinence
There are limited surgical options for fecal incontinence, and the options presented will be dependent on your dependent on your surgeon’s experience and preferences. Obstetric injuries (from vaginal delivery) are the most prevalent sphincter injuries amongst women. Surgery to restore the muscle to its original anatomical form is often performed at the time of injury. A 2012 systemic review into to assess long term outcomes of sphincter repair reported that initial outcome was subjectively reported as “good” but declines were common in long term follow-up. Sphincter repair on its own may not be sufficient and should be followed with a program of PFMT to rehabilitate the newly repaired muscle.
If your condition is connected to Pelvic Organ Prolapse or Rectocele, you should review the advice given on the POP page with regards to the treatments available for those conditions. If you condition is not connected to POP, there are just two surgical options listed below. Remember that all surgeries carry risks. You should work diligently at all conservative options before considering surgery. Your doctor or healthcare provider can guide you to your best options.
Sacral Nerve Stimulation (SNS) For the Treatment of Fecal Incontinence
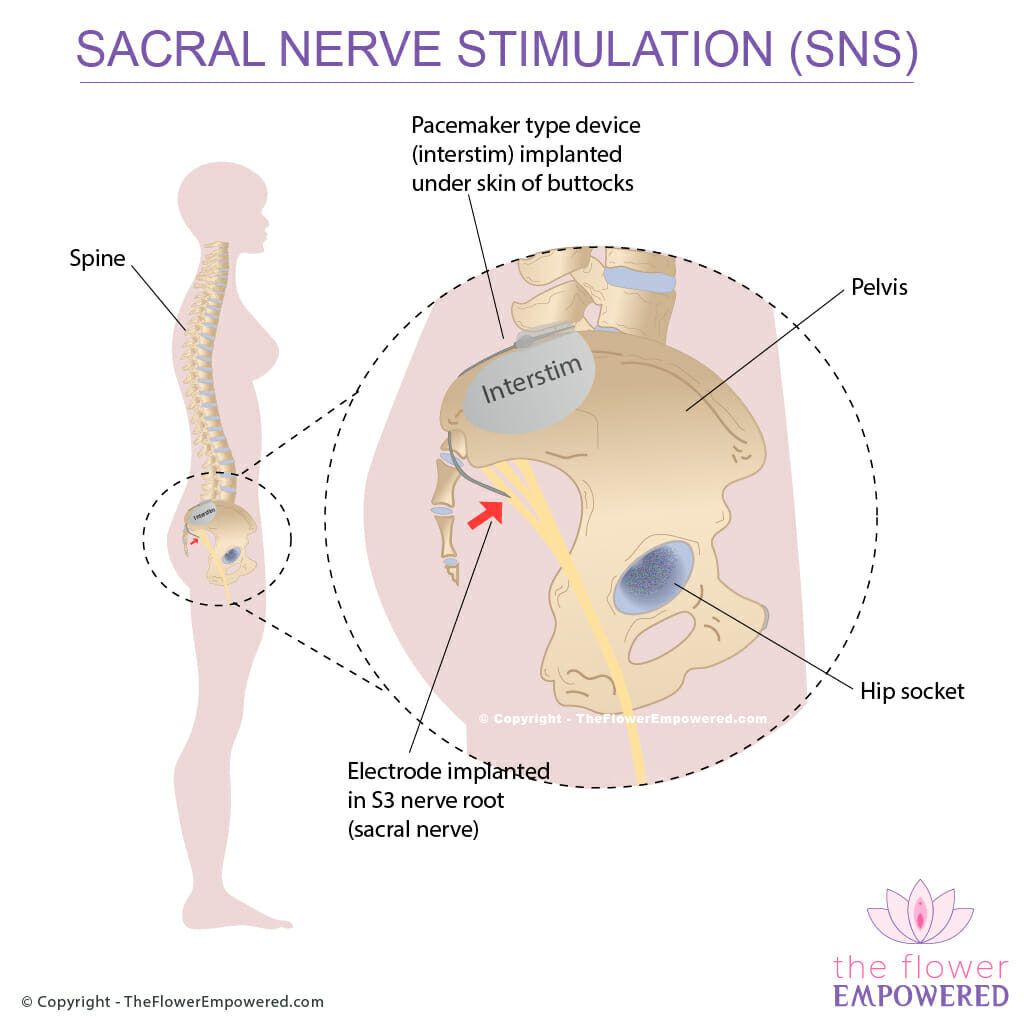
Sacral Nerve Stimulation (SNS) is the most invasive treatment available for fecal incontinence. It involves implanting a pacemaker type device under the skin of the buttocks with an electrode that is fed into the S3 sacral nerve root. This treatment is also used as a treatment for overactive bladder which you can read about on the urinary incontinence surgical treatments page.
The exact mechanism that makes this an effective treatment is not understood. However, studies have demonstrated improvements in anal resting and squeeze pressures and changes in rectal sensitivity.
The device is 2 inches wide and quarter inch thick. Battery is expected to last 5 years, however, the manufacturer emphasises that the more you use it, the quicker it will run out. Changing the battery involves a subsequent surgery. You can have a two week trial before device implantation which is quite unique. During this trial period, you will have probes going into your sacral nerve but will have a small device strapped to your waist instead of the implant.
A Cochrane review in 2015 evaluated the available studies into SNS for FI and found that it was unsuitable for those with constipation.
Other Surgical Alternatives to Treat Fecal Incontinence
There are a number of other surgical alternatives for repair of the anal sphincter, however most of them have higher risks or are experimental. One treatment, the graciloplasty, involves taking the Gracilis muscle from inside the leg and rotating it to come up and wrap around the sphincter. The muscle is then fitted with a nerve stimulator to increase the tone for sphincter contractions. The surgery is complicated and, according to a 2013 study, is no-longer performed in the US due to the unavailability of the nerve stimulater.
Other treatments involve implantation of inflatable devices or magnets to act as an artificial urethral sphincter. The efficacy of these devices has yet to be confirmed with long term studies.
Set Appropriate Expectations Before Undergoing Surgery
It is important to have realistic expectations if you are going for surgery, and to ensure that both you and your surgeon are on the same page. Successful surgery according to you might not be the same as successful surgery according to your surgeon. Studies into the surgical treatment of FI typically measure success either as object cure rate, subjective cure rate or a combination of the two. Within a single study, the objective and subjective cure rates can vary greatly.
A good example of this is this study from 2003 evaluating the outcome of implantation of artificial anal sphincters into 25 people. According to the scoring system used to assess objective cure, of the 19 patients for whom the sphincter was successfully activated, all were 100% continent. However, 36.8% of the patients reported emptying difficulties with some requiring regular enemas and laxatives to allow for satisfactory emptying meaning that subjectively the surgery could not be considered 100% successful for those patients.
Conservative Treatment Fecal Incontinence
Having viewed the invasive (surgical) treatments for Fecal Incontinence, you may also be interested in the conservative (non-surgical), which you can get to from the button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.