Vaginismus is believed to impact between 5% and 17% of women1
What is Vaginismus?
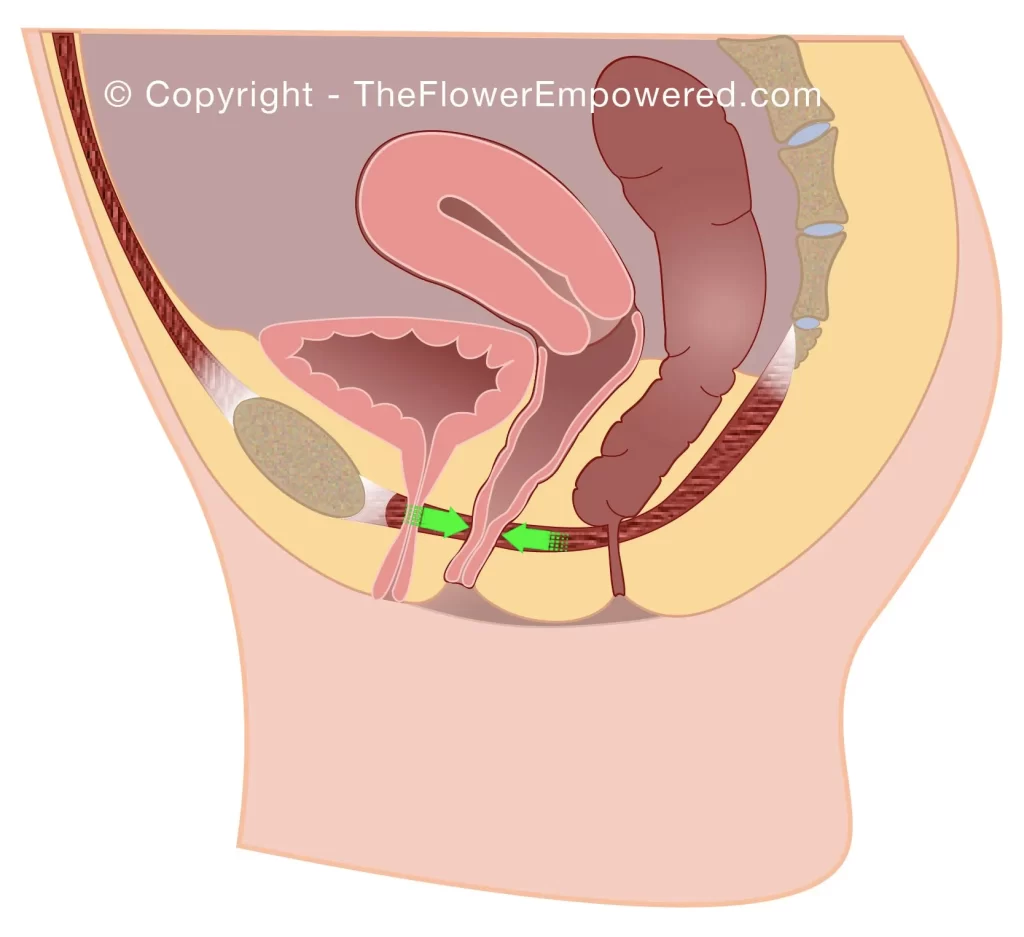
Vaginismus is a condition where the vaginal muscles involuntarily spasm interfering with the use of tampons, period cups, gynecological exams and sexual intercourse. The key word is involuntarily, meaning that you have no control over the contraction of the pelvic floor. Many women with vaginismus reporting hitting a “wall” when trying to use a tampon or to have penetrative sex. Vaginismus is a form of pelvic floor dysfunction.
What Are the Different Types Vaginismus?
There are three different types of vaginismus: .
Primary, where vaginal penetration has always been difficult or impossible due to contracted pelvic floor muscles. This type of vaginismus is usually discovered in puberty or early adulthood.
Secondary, where penetration was once possible but is no longer achievable without great difficulty and pain due to tight/contracted pelvic floor muscles. This can happen due to pelvic surgery, menopause, radiotherapy, infections, sexually transmitted diseases or other factors. This type of vaginismus is generally discovered in mid to late adulthood, although it can happen at any time.
Spontaneous, where vaginismus is occurs in an isolated occasion. This can be during penetration or when using vaginal weights. This type of vaginismus is often experienced without pain. It can happen at any point but is not considered true vaginismus as it is not chronic and can generally be resolved quickly and without extended treatment.
How Is Vaginismus Diagnosed?
Vaginismus is diagnosed by performing a gynelogical exam. Do not attempt to self-diagnose. Many women experience some difficulty and pain the first time they try use a tampon. Almost all women will experience some pain when they have sex. These are normal experiences and they do not indicate that you have vaginismus. Both inserting tampons and having penetrative sex become easier with time. If you find that you have tried multiple times but without success, make an appointment with your gynecologist or speak with your doctor.
Pain can induce fear which can make it harder to relax. A 2021 study found that women with vaginismus have a lower threshold of pain, and the pain threshold decreases in higher grades of vaginismus2. A 2020 systemic review of 60 randomized clinical trials found that mind-body therapies were associated with improved pain3. If you have been diagnosed with vaginismus, yoga, relaxation and meditation can help you to control pain as you work to overcome the condition.
How Is Vaginismus Severity Graded?
When you have your gynaecological assessment, the doctor will assign a grade to your vaginismus based on what is found on examination. It is important to relax during the examination as much as possible. Meditation and breathing techniques can be helpful in calming your nervous system allowing for the examination to proceed.
What Happens During the Gynaecological Exam?
Before any gynaecological exam, you should explain to your concerns regarding vaginismus. This will ensure that the doctor is aware that you may have vaginismus. You will sit on a special chair with leg supports. These are intended to help you to relax. In some cases the doctor may give you a mirror to look at your vulva and they will explain the different parts and talk you through the exam before they begin.
For a standard gynecological exam, a speculum is often used to gently open the vaginal passage allowing the doctor to look inside to see if everything looks healthy. If you have vaginismus, they can begin by first trying to use a q-tip to see if you can relax for that. If you are comfortable with the q-tip, they may ask you to try insert one or two of your own fingers to see if that is ok for you.
If the q-tip and fingers are ok, they can try to perform the exam using a pediatric (small size) speculum. They will insert the speculum and open it slightly so they can perform the check-up. They will grade the severity of your vaginismus based on this exam. Grading is based on the Lamont-Pacik classification system4.
Grades of Vaginismus
- Grade 1: Spasm of the pelvic floor that can be relaxed by reassurance – patient can relax for exam.
- Grade 2: Generalised spasm that does not subside with reassurance – patient cannot relax for exam.
- Grade 3: Stronger spasm that causes lifting of buttocks to avoid examination.
- Grade 4: Severe spasm with retreat and legs snapping closed to avoid examination.
- Grade 5: Severe spasm with additional visceral symptoms such as trembling, shaking, extreme anxiety, crying, screaming, sweating, palpitations, hyperventilation, nausea, or vomiting.
The defined grade is believed to be linked to the grade of vaginismus with one 2021 study concluding that Patients should be notified that as the grades of vaginismus progress, the duration of the treatment may extend, and its success may decrease, the requirement for mechanical dilators will increase in the advanced grade, and the grade may progress as the application period for treatment is delayed5.
Products for Management of Vaginismus
There are many products that can be used in the management vaginismus. We have include some of those products below. You should speak with your pelvic floor physiotherapist or gynecologist before using these products. Reviews of these products will be covered on our YouTube channel. If there is a specific product that you would like to see reviewed, just get in touch and we will review. Note that these products have affiliate links. Should you choose to purchase them, we will make a small commission.
Treatment Options for Vaginismus
Like most symptoms of pelvic floor dysfunction, the treatment for vaginismus falls into one of two categories; conservative (non-surgical) and invasive (surgical). Surgical options are generally only advised for once conservative options have been tried unsuccessfully for an extended period. For more information on the various treatments offered you can view the sexual dysfunction treatments by clicking on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
Explore the Other Types of Sexual Dysfunction
Having reviewed this information on vaginismus, you may also be interested in exploring dyspareunia. You can do that from here:
References
- Pacik PT, Geletta S. Vaginismus Treatment: Clinical Trials Follow Up 241 Patients. Sex Med. 2017 Jun;5(2):e114-e123. doi: 10.1016/j.esxm.2017.02.002. Epub 2017 Mar 28. PMID: 28363809; PMCID: PMC5440634.
- Eserdag S, Sevinc T, Tarlacı S. Do women with vaginismus have a lower threshold of pain? Eur J Obstet Gynecol Reprod Biol. 2021 Mar;258:189-192. doi: 10.1016/j.ejogrb.2020.12.059. Epub 2021 Jan 6. PMID: 33450709.
- Garland EL, Brintz CE, Hanley AW, Roseen EJ, Atchley RM, Gaylord SA, Faurot KR, Yaffe J, Fiander M, Keefe FJ. Mind-Body Therapies for Opioid-Treated Pain: A Systematic Review and Meta-analysis. JAMA Intern Med. 2020 Jan 1;180(1):91-105. doi: 10.1001/jamainternmed.2019.4917. PMID: 31682676; PMCID: PMC6830441.
- Pacik PT, Babb CR, Polio A, Nelson CE, Goekeler CE, Holmes LN. Case Series: Redefining Severe Grade 5 Vaginismus. Sex Med. 2019 Dec;7(4):489-497. doi: 10.1016/j.esxm.2019.07.006. Epub 2019 Aug 28. PMID: 31473152; PMCID: PMC6963107.
- Kiremitli S, Kiremitli T. Examination of Treatment Duration, Treatment Success and Obstetric Results According to the Vaginismus Grades. Sex Med. 2021 Oct;9(5):100407. doi: 10.1016/j.esxm.2021.100407. Epub 2021 Aug 5. PMID: 34364175; PMCID: PMC8498957.