2020 Study Concludes Physiotherapy Is an Effective Method of Conservative FI Treatment in Women1
Conservative Treatments for Fecal Incontinence
When it comes to non-surgical treatments for fecal incontinence, the primary treatment is pelvic floor muscle training (PFMT). Due to fecal incontinence involving the gastrointestinal tract, sometimes treatments can focus on diet, microbiome or medication. You should always speak with your doctor or healthcare provider if you have symptoms. They will know which specialists are best to help you. Often, the approach is multidisciplinary, with multiple doctors making assessments and offering treatments. This page will summarize the non-surgical treatments.
Pelvic Floor Muscle Training (PFMT)
Traditional pelvic floor muscle training is one of the primary conservative treatments for fecal incontinence. PFMT involves exercising pelvic floor muscles to restore muscle strength and function. These exercises are often called Kegels – named after Dr. Arnold Kegel who first identified the importance of strengthening these muscles to maintain a stable vaginal canal. In the case of anal sphincter weakness, particular attention may be given to contractions involving the anal sphincter.
Consistency and variation with is key when working to improve the strength of your pelivc floor. You can sign up for our 30 day challenge to get an insight into what varied training looks like. When you sign-up, you will get access to a bonus video that goes through the steps to perform a complete Kegel while also making a short self-assessment of your ability to contract your pelvic floor. This is not intended to replace a proper assessment by your healthcare professional.
Bowel Retraining
Bowel retraining is where you “positively reprogram” your defecation through a number of practices that help to reinstate good bowel habits. An important part of bowel retraining is taking a baseline to establish where you are right now, and then tracking your progress over time. This is done under the guidance of your healthcare provider (typically advanced practice nurses2). It is not advised to undertake bowel retraining without medical supervision.
Is PFMT Needed if I’m doing Bowel Retraining?
Pelvic floor muscle training plays an important role in bowel retraining, as contraction/relaxation of the anal sphinter is needed to coordinate holding and emptying. Your doctor will likely refer you to a pelvic floor physical therapist to help you with this training. Your physiotherapist may use biofeedback as well as ultrasound to directly see the activation of the pelvic floor. In some cases, a three dimensional pelvic ultrasound machine may be used to get a more accurate picture of what is happening through the entire pelvic floor.
Additional Conservative Treatments
1. Diet and Nutrition
When it comes to Fecal Incontinence, it is almost as important to assess your diet, which is one of the reasons we included the additional question regarding the consistency of your normal poo in the severity test. If your “normal” poo leaves you with constipation or loose stools/diarrhoea, it is imperative that you make changes to your diet. Constipation and diarrhoea have a detrimental impact on your pelvic floor and can lead to FI if they are chronic. Look for a local nutritionist in our Specialist directory. Let us know if you fail to find someone in your area and we will try to help.
When you consider that your diet plays a major role in digestion and that constipation and diarrhoea increase your risk of developing FI, you should take your diet seriously. Probiotics can help to boost your microbiome with lots of healthy bacteria. It is important to have your bloods checked to ensure you are sufficient in essential vitamins and minerals. A good nutritionist can advise you on the best diet for your specific condition.
2. Weight and BMI
Did you know that for every additional unit increase in your BMI, your risk of developing urinary incontinence increases by 1%? In fact, obese people have a double the risk for developing urinary incontinence. The severity of incontinence is also more severe if you are obese and lowering the BMI has been shown to lower the severity. Given that up to 24% of women who suffer urinary incontinence will also suffer fecal incontinence, you should strive to keep a healthy BMI.
3. Food and Bowel Diary
Your pelvic health specialist or nutritionist may ask you to keep a diary of your food intake and bowel movements over a couple of months to identify your patterns. You can do this using pen and paper or alternatively use an app such as Tummy Lab which was created to track Irritable Bowel Syndrome (IBS) and other digestive issues. In this app, you can track the food you eat, your bowel movements, your symptoms and many other data-points that may be of interest. Your pelvic health specialist might suggest bowel retraining if your pattern of movements is highly irregular.
4. Training Other Muscle Groups
Your pelvic floor has relationships with surrounding muscles. In recent years, Biomechanists, structural integrators, movement therapists and yoga teachers have been expanding pelvic floor rehabilitation programs to include other key muscle groups that have a direct relationship to the pelvic floor (such as the diaphragm, core and gluteus muscles). By working on a range of functional movements, in combination with Kegels, the pelvic floor can become more stable. This should help to improve your overall fitness level as well as reducing the symptoms of your FI.
5. Posture and Alignment
Posture and alignment impact the stability of your pelvic floor and should be assessed as part of your rehabilitation. Your connective tissue (fascia) holds your body in its normal posture. Advancements in fascial research has created a much clearer understanding on how load is distributed through your body. When you view your pelvic floor muscles in isolation, you are viewing just a small part of the puzzle. Working with a myofascial release therapist or structural integrator is a wonderful addition to your rehabilitation.
6. Managing Your Mental Health
The psychological aspect to fecal incontinence is substantial. The condition can leave you afraid to even leave home, mapping toilet locations when you do so as not to get caught unawares. Self-esteem greatly suffers and depression and anxiety are often reported with the severity of depression increasing along with the severity of FI. It is imperative that you seek help as soon as possible. Speaking to a therapist can help you deal with the negative impact of living with FI. Meditation can also be of benefit as you undertake your rehabilitation. Please realise that you are not alone. You can connect to others that have FI in our community.
7. Group Training
A randomised study that evaluated the effects of PFMT for stress incontinence showed that those doing group training showed significant improvement over those training at home alone. With FI, you are probably less reluctant to go outside, but the sense of community and support when you train with others might boost your self-esteem and prevent you from feeling isolated. If your pelvic health physiotherapist does not offer a weekly group session, try to find a pilates, yoga or hypopressive class focusing specifically on training the pelvic floor.
8. Other Lifestyle Changes
An important lifestyle choice connected to fecal incontinence relates to anal sex. A 2016 study which included 2070 women concluded that anal intercourse can be a contributing factor with anal incontinence. In the book, anal sex is explored from the perspective of the pelvic floor as there are some considerations that can help to reduce the impact on your pelvic health if anal sex is your thing. You should definitely pause the activity if your incontinence is severe and take time to heal before resuming.
Medication for Fecal Incontience
Many medications can aggravate the digestive system thus changing the consistency of your poo. It is important to carefully consider everything that goes into the mouth as it will eventually make some level of an appearance at the other end of your digestive pipe. Medication for treatment of FI tends to be for symptom control and is typically used over the short term. If loose stools or diarrhoea are contributing, drugs like Imodium may be offered. If constipation is contributing, bulking laxatives such as Psyllium may be offered. Aside from these medications, which focus on changing the consistency of your poo, there are one or two other medications that can be given. Amitriptyline can be used to decrease rectal contractions. A low dose of Clonidine can be used to reduce rectal sensation and urgency.
All medications come with side effects and often treat the symptom and not the root cause. Speak to your doctor or healthcare provider to find out if medication might be right for you.
Pessaries, Anal Plugs and Electrical Stimulation
If your condition is connected to Pelvic Organ Prolapse or Rectocele, you should review the advice given on the POP page with regards to the treatments available for those conditions. If you condition is not connected to POP, there are some other alternatives listed below. Pessaries and anal plugs are for management of the condition rather than a permanent cure. Your doctor can advise if these treatments are right for you.
Anal Plugs and Pessaries
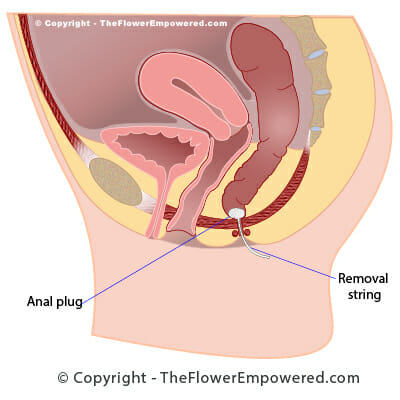
Pessaries and Anal Incontinence plugs are devices which you will insert into the body. Pessaries for fecal incontinence can only be used by women due to their placement within the vaginal passage. They are similar to the pessaries used for pelvic organ prolapse but with more pressure on the back wall to mimic the function of the puborectais muscle by making a kink in the rectum.
Anal plugs can be used by both men and women. The are designed to function in a similar way to a tampon, but for anal insertion. Anal plugs are made from an absorbable foam covered by a thin film that dissolves when it comes in contact with bodily fluids. Once the film has dissolved, the absorbable material expands to seal the rectum. The foam itself is porous to allow gas to pass through. Like a tampon, the plug has to be passed sufficiently high into the rectum for correct and comfortable positioning. If the plug expands in the lower part of the rectum, it can be extremely uncomfortable while adding unnecessary pressure to the internal and external sphincters.
A 2005 study found that anal plugs can be “difficult to tolerate, however, if they are tolerated, they can be helpful in preventing incontinence”. Another study from the Nursing Times (2008) found that patient uptake was low until correct placement was demonstrated in a clinic setting. If used correctly, the anal plug can be useful to manage the symptoms of FI while working on pelvic floor rehabilitation.
.
Anal Plug to Prevent Fecal Leakage
Electrical Stimulation for Fecal Incontinence
Transcutaneous Prosterior Tibial Nerve Stimulation (TPTNS) is stimulation of the tibial nerve with skin surface electrodes. This treatment is the least invasive of the nerve stimulation options for FI. The treatment is preformed by placing two skin electrodes above and below the ankle where the tibial nerve is located.
Whereas PTNS (Prosterior Tibial Nerve Stimulation) is performed in clinic by a doctor, TPTNS can be preformed at home using an NMES device. This is the same device that is used to perform electrical stimulation of the sphincter with an anal probe, you just connect skin electrodes instead. There have been limited studies into TPTNS, however, completed studies have shown that it can relieve the symptoms of fecal incontinence. You should only use this treatment if advised by your doctor.
Transcutaneous Prosterior Tibial Nerve Stimulation (TPTNS)
Invasive Treatments for Fecal Incontinence
Having reviewed the non-surgical treatments for fecal incontinence on this page, you may be interested in exploring the invasive options which include some minimally invasive options and some surgeries. Surgical options are generally only advised for once conservative options have been tried unsuccessfully for an extended period. For more information on the various treatments offered in these two categories, click on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
References
- Mazur-Bialy AI, Kołomańska-Bogucka D, Opławski M, Tim S. Physiotherapy for Prevention and Treatment of Fecal Incontinence in Women-Systematic Review of Methods. J Clin Med. 2020 Oct 12;9(10):3255. doi: 10.3390/jcm9103255. PMID: 33053702; PMCID: PMC7600070.
- Bentsen D, Braun JW. Controlling fecal incontinence with sensory retraining managed by advanced practice nurses. Clin Nurse Spec. 1996 Jul;10(4):171-5. doi: 10.1097/00002800-199607000-00004. PMID: 8900792.