Uterine Prolapse
A uterine prolapse (Utero-Vaginal) occurs when the ligaments of the uterus are stretched due to weakness in the pelvic floor resulting in the uterus being pushed or pulled into the vaginal passage. Cystocele and Rectocele can also lead to development of a uterine prolapse due to the pulling on tissues. With a uterine prolapse, you may feel the uterus bulging into the vagina. Uterine prolapse is measured in stages ranging from stage 1 which is a minor prolapse, to stage 4 which is complete prolapse. It is very important to begin pelvic floor muscle training as soon as possible to regain the strength in your pelvic floor and lessen the symptoms of your prolapse.
Because this type of pelvic organ prolapse causes the womb to drop into the vagina, the bowel and bladder can be impacted as the uterine support ligaments play a role in the overall stability within the pelvis. Issues with urinary incontinence, fecal incontinence and sexual dysfunction can occur with uterine prolapse. With a full uterine prolapse, the entire uterus is outside the body. If you believe you may have a prolapsed, you should see your doctor or pelvic floor physical therapist (physiotherapist).
Grades of Uterine Prolapse
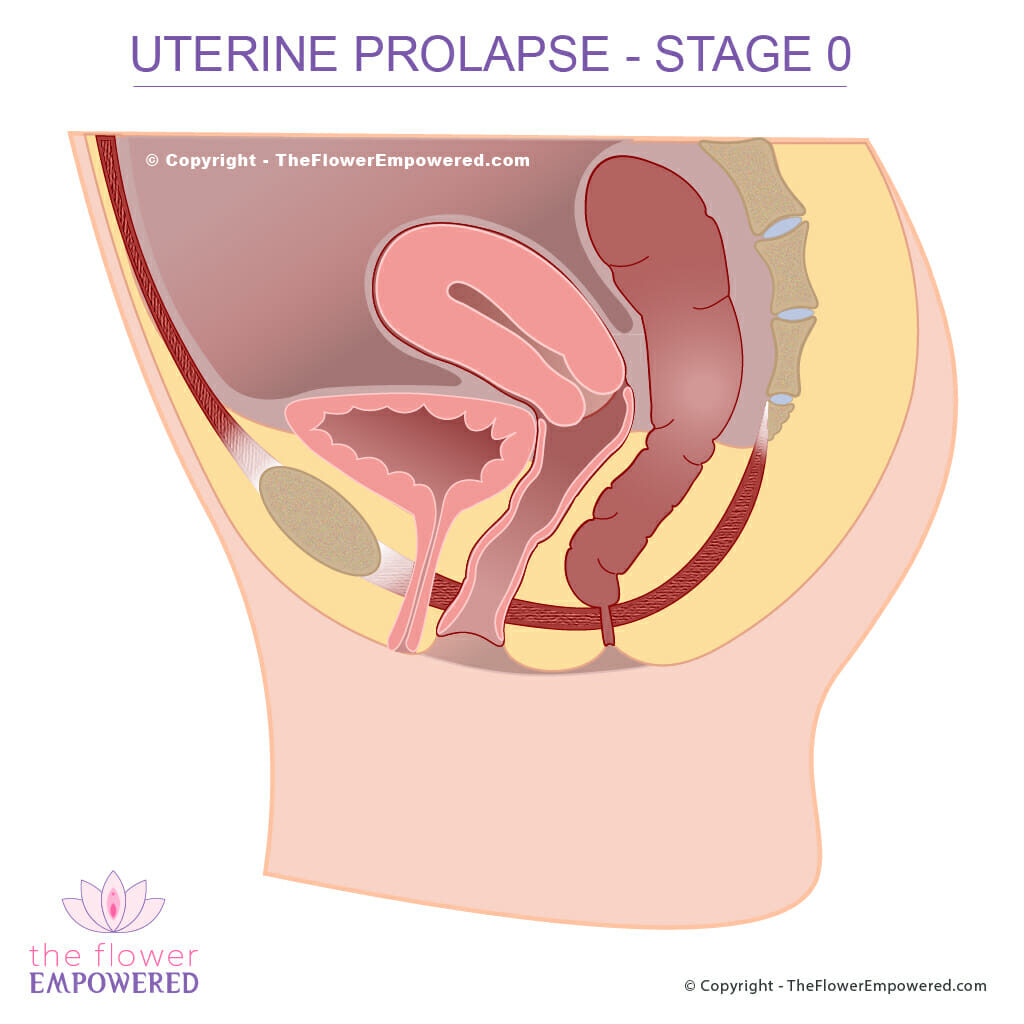
Bear in mind when looking at these images that they show the prolapse when under increased intraabdominal pressure. Without an increase in intraabdominal pressure, the organs and tissues do not generally bulge in the same way. In the case of severe prolapse, the bulge may be present at all times.
Stage 0 (No Prolapse)
Stage 1 (Mild Prolapse)
Stage 2 (Moderate Prolapse)
Stage 3 (Severe Prolapse)
Considerations When You Have Uterine Prolapse
As with all prolapses, it is important to maintain good bowel function and to prevent straining. You can do this by ensuring you eat sufficient fiber and stay hydrated. A weak pelvic floor will sit lower than normal so pelvic floor muscle training is important when you have prolapse. Hypopressive breathing exercises can also be helpful as they work to enhance the relationship between the diaphragm and pelvic floor.
Make sure to avoid constipation as the bearing down when constipated can stretch the tissues further causing a worsening of your prolapse. You can find many videos on our YouTube channel giving tips on preventing constipation and demonstrating pelvic floor exercises and hypopressive techniques that if practiced consistently over time, will help to lessen your symptoms and improve the grade of your pelvic organ prolapse1.
Uterine prolapse is heavily impacted by the ligaments of the uterus, which form a ring of support around the cervix (neck of the womb). Pessaries can be very helpful in bolstering this ring of support, even in advanced stages of prolapse. One study reported success rates of up to 62% when using pessaries in patients with stage 3 and 4 prolapse2. You can find out more about pessaries in the conservative (non-invasive) treatment page for prolapse.
Treatment for Uterine Prolapse
Uterine Prolpase treatments, like those of the other forms of prolpase, are either conservative (non-surgical) or invasive (surgical). Surgical options are generally only advised for severe uterine prolapse (grade 3 or 4). For more information on treatments, click on the relevant button below. If you did not find what you were looking for, you can search this site using the search bar at the bottom of the page.
Explore the Other Types of Pelvic Organ Prolapse
Having reviewed the Uterine Prolapse, you may be interested in exploring the other types of prolapse. You can do that from here:
References
- Bernardes BT, Resende AP, Stüpp L, Oliveira E, Castro RA, Bella ZI, Girão MJ, Sartori MG. Efficacy of pelvic floor muscle training and hypopressive exercises for treating pelvic organ prolapse in women: randomized controlled trial. Sao Paulo Med J. 2012;130(1):5-9. doi: 10.1590/s1516-31802012000100002. PMID: 22344353.
- Jones KA, Harmanli O. Pessary use in pelvic organ prolapse and urinary incontinence. Rev Obstet Gynecol. 2010 Winter;3(1):3-9. PMID: 20508777; PMCID: PMC2876320.